INTRODUCTON
Fracture of the orbital floor is a common injury accompanying mid-face traumas. Its incidence ranges from 18 to 50% of all cranio-maxillofacial traumas, depending on the geographic region, injury mechanism, and study population.1,2 Although the eyeball is well protected by the strong orbital rim and thin orbital floor, and the medial wall acts as a shock absorber, there is a high incidence of associated ocular injuries after orbital trauma, ranging from 22 to 76% in reported series.3,4 Failure of prompt recognition and treatment of these injuries may result in significant functional and cosmetic problems. In bone repair and orthopedic therapies, there is an increasing demand for solutions, driven by aging demographics, increased awareness, globalization, technological and product advances, increasing number of sport injuries, and improved patient care strategies. However, ideal solutions for bone diseases (defined as a disordered or incorrectly functioning bone, part, structure, or whole skeletal system of the body, resulting in a harmful, depraved, or morbid condition) have eluded us for many years and continue to pose a significant challenge for orthopedics, trauma, and maxillofacial surgeons. Many of these diseases have great influence over the quality of life and could be fatal in extreme cases. To address this need to improve awareness, prevention, and treatment, and to eventually preserve our quality of life, the United Nations (UN) and the World Health Organization (WHO) declared 2000–2010 as the Bone and Joint Decade.5
The face should have the harmonious symmetrical relationship between the paired and unpaired facial structures that form our first impression of what a person is like. The eyes, their color, three-dimensional position, and synchronous movement are a major contribution to this overall picture. Eye position and movement should be symmetrical and are important from an aesthetic point of view.6
Fracture in and around the orbit vary from linear fractures to complex craniofacial injuries involving the orbital rim and several orbital walls. Blow out fracture of the orbit most commonly involve the floor and the medial wall.7
Trauma to the orbit can result in considerable facial deformity and at the same time affects both vision and the nervous system of the face.8–12 The etiology can be traffic related 77.7%, violence related 10%, or work related and other reasons 13.3%.13 Orbital floor fractures have specific clinical attention for several reasons. Failure to recognize and treat them early may result in severe sequelae. However, despite surgical intervention, orbital floor fractures are associated with risk of persisting sensibility disorders, enophthalmos, and permanent diplopia.14
Autogenous bone grafts are the gold standard for reconstruction of maxillofacial defects. Autogenous bone becomes osseointegrated and vascularized at its site of implantation, which decrease the chances of infection, displacement, and foreign body reaction compared with alloplastic implants. The drawbacks include the harvest time, donor site morbidity, graft resorption, modeling changes, and harvest volume limitations.15
The clinician must choose the site of bone harvest wisely, considering the nature of the reconstruction and volume requirements. Autogenous bone can be harvested from multiple sites, including the calvarium, tibia, anterior ileum, posterior ileum, rib, sternoclavicular joint, zygoma, mandible, and so on.16,17
Autologous bone grafting dates back to the ancient Egyptian times, and the modern use and scientific study of this “gold standard” implant material for bone regeneration began in the early 19th century.18 When a bone graft is required to repair a defect, autogenous bone graft is frequently performed during surgery as it possesses the three main ideal traits, identified by Marshall Urist, for bone healing.16,17
PATEINTS AND METHODS
A total of 15 patients were enrolled in this study, all with orbital floor fracture, of which 10 of them were having pure blow-out fractures and the other 5 patients had impure blow-out fractures. All had underwent primary surgical reconstruction of the orbital floor by autogenous anterior iliac crest within 2–14 days after injury.
Patients’ age ranged between 10 and 36 years, and there were 12 males and 3 females.
Inclusion criteria
Patients with the following criteria were included in the study:
-
Patients with orbital floor fractures regardless their age or gender
-
Preoperative computed tomography (CT) scanning in coronal, sagittal, and axial projection verifying fracture pattern
-
Orbital floor defect of more than 50% confirmed by CT scanning
-
Patients with enophthalmos
-
Patients with diplopia
-
Disturbances in eye movement.
Exclusion criteria
Patients with the following criteria were excluded from the study:
-
Serious general disease
-
Grossly displaced zygomatic or maxillary fracture
-
Pan facial fracture
-
Unfit for surgery
-
Refused to participate.
Measuring of Enophthalmos
The mean preoperative enophthalmos was about 4 mm measured by a ruler from the lateral orbital rim of the injured eye to the most anterior projection of the globe in comparison to the intact contra-lateral eye.
RESULTS
Sex and age of patients
There were 12 males (80%) and 3 females (20%) with a male to female ratio of 4:1 (Figure 1).
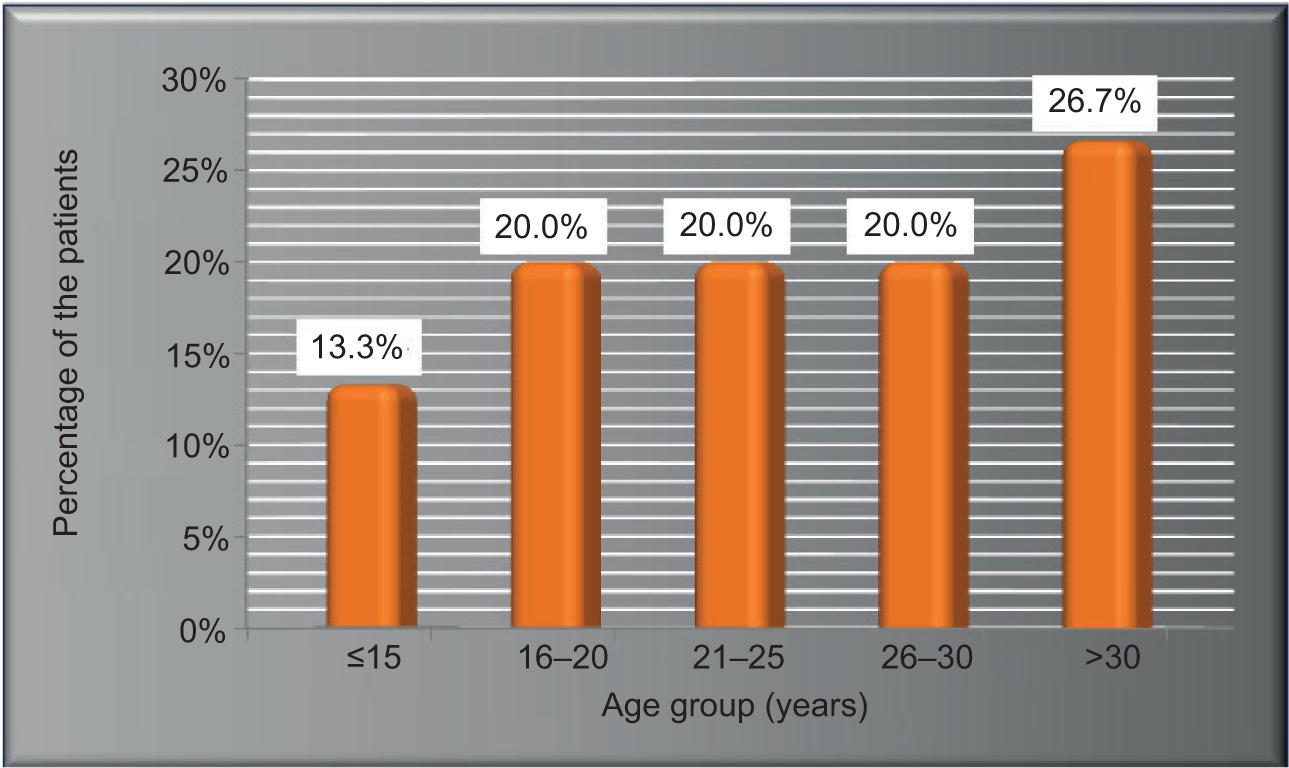
The age distribution of the patients revealed a mean age of 24.9 ± 2.1; Furthermore, two patients (13.3%) were aged ≤15 years, three patients (20%) belonged to each of the next three age groups, 16–20, 21–25, and 26–30 years, and four patients (26.7%) were aged >30 (Figure 2).
FIGURE 1. Gender distribution of the patients, (N = 15, Male to female ratio = 4:1).
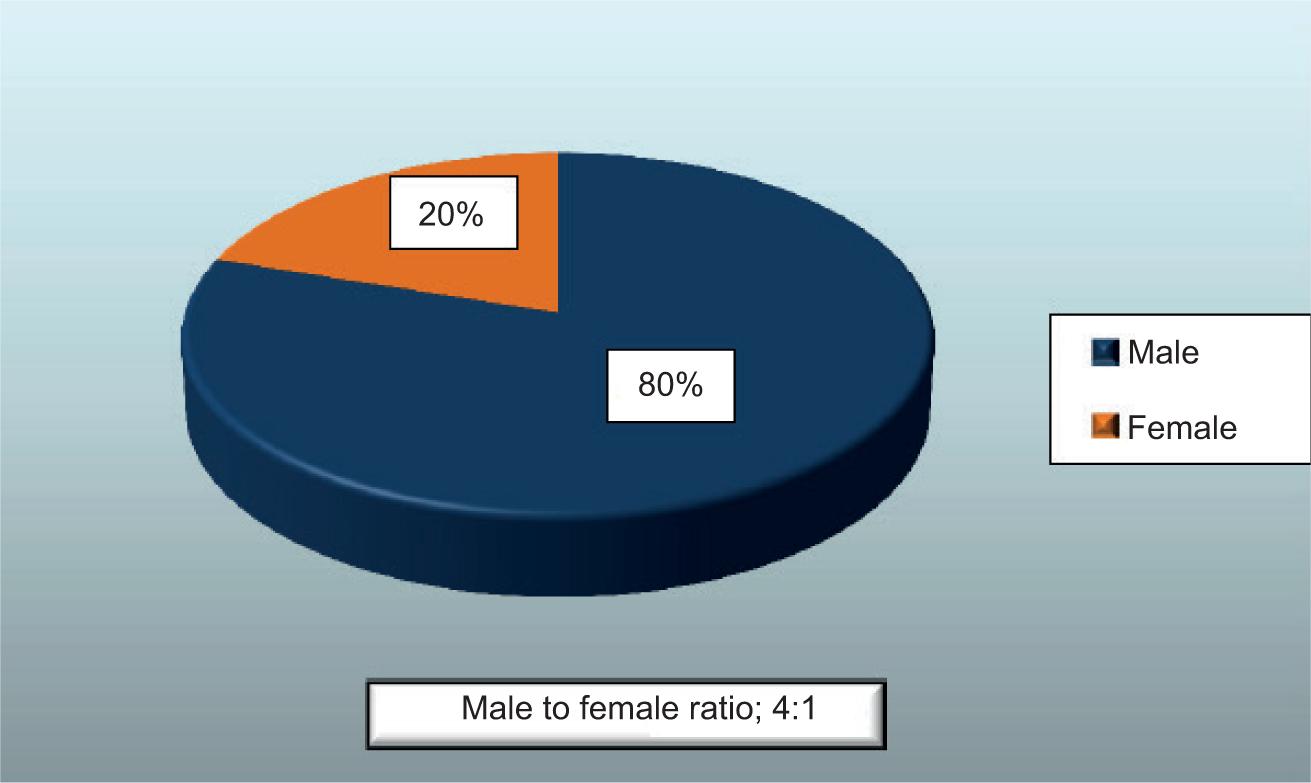
FIGURE 2. Age distribution as percentages of the studied group, (N = 15).
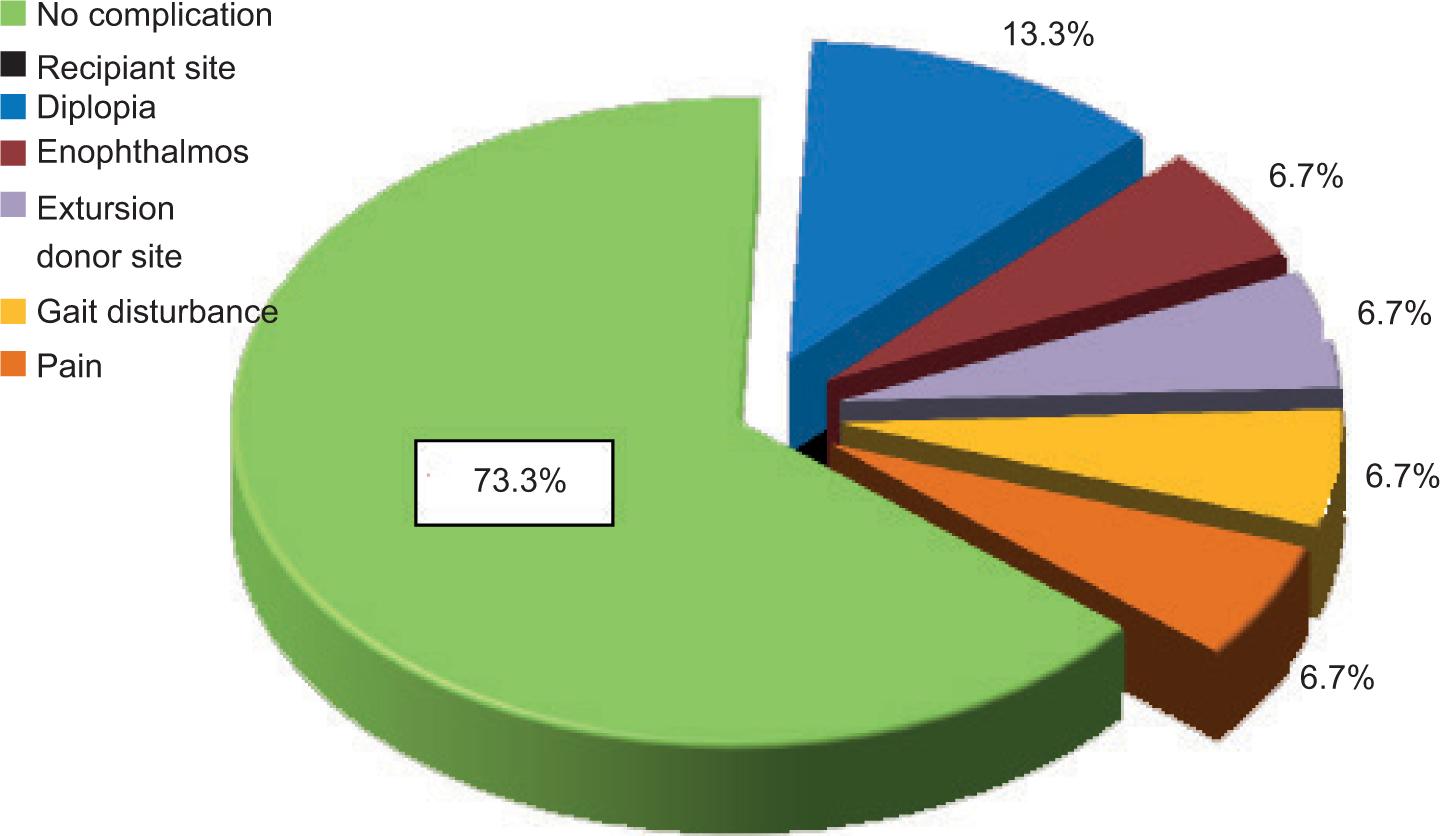
Postoperative complications
As shown in Table 1 and Figure 3, 11 patients (73.3%) had no complications, while postoperative complications had been found in only 4 patients (26.7%) at the recipient site; two patients (13.3%) had diplopia, one patient (6.7%) had enophthalmos, and one patient (6.7%) had extrusion. Furthermore, at the donor site, one patient had pain and another one had gait disturbances, which persisted for more than a week. Pain and gait disturbance relieved within 1 month after treatment with analgesia and physiotherapy, respectively, and the patient appeared normal.
TABLE 1. Postoperative complications of patients.
| Complication | No. of patients | % |
|---|---|---|
| Recipient site | ||
| Persistent Diplopia | 2 | 13.3 |
| Enophthalmos | 1 | 6.7 |
| Extursion | 1 | 6.7 |
| Donor site | ||
| Pain | 1 | 6.7 |
| Gait disturbance | 1 | 6.7 |
FIGURE 3. Proportions of postoperative complications at recipient and donor sites.
DISCUSSION
Patient population
Our study yielded a male to female ratio of 4:1 patients, and the highest risk group was young males. Young male population made up the highest orbital floor fracture and for trauma in general, presumably because of the propensity of that group to engage in high-risk activities which corresponded to the findings of the study by Tong et al. in 2001.18
Reconstruction material
Various materials have been used to replace the damaged bone sites on maxillofacial region for reconstructive and cosmetic reasons. Fracture of the thinnest areas of orbital walls by mechanism of increased intraorbital pressure or buckling force requires surgical treatment with one of these materials. The goal of the operation is to restore the appropriate position of the globe inside the bony orbit.19
There are several theories on the formation of traumatic and postoperative enophthalmos. Enlargement of bony orbit, loss of ligament support, post-traumatic fat atrophy, and scar contracture are some of the mechanisms that have been defined so far. Choosing the material to span the defect and determining the volume to be inserted are still difficult and controversial step in reconstruction. Autogenous grafts have been used to restore orbital anatomy for many years. The application of split calvarial bone, which is a membranous structure, is known to be advantageous over endochondral bone; but unfortunately, harvesting the cranial bone graft increase the operating time, and due to close proximity of the surgical field, it cannot be performed simultaneously with orbital floor approach. The human cranium cannot reach its terminal thickness before the age of 17, and for this reason, dural tear, meningitis, and epidural hematoma are serious and life-threatening donor site complications, especially in children. Various types of synthetic materials are being used successfully for orbital floor defect; however, low potential for biocompatibility and higher infection rates are still a problem, despite their easy application and decreased donor site morbidity.20,21
Autogenous iliac crest bone graft was the first material used to reconstruct the internal orbital walls and have been the gold standard to provide a framework for facial skeleton. Autogenous iliac crest ensures the establishment of bony continuity across the defect and become incorporated into the defect as a new bone. Larger volume of graft material necessary for complex reconstruction are likely to be better tolerated than equal volume of alloplastic material. The other advantage is its relative resistance to infections. The lack of host response, biocompatibility, osteoconductive and osteoinductive properties, the lack of concern against late extrusion or donor site morbidity, variable graft resorption, limited ability to contour are some of the disadvantages.22,23
Extrusion
Only 1 case out of 15 shows a postoperative extrusion due to which no method of fixation is applied to the piece of graft. Although there are seven cases which present with no method of fixation, there is no history of extrusion.
Graft failure
No graft failure or rejection by host was seen in this group, and this finding correlates with that of Roncevic et al.24
Donor site complication
Complications following iliac crest bone grafting are not infrequent, and the most common complications of bone harvest from the anterior iliac crest are postsurgical pain, gait disturbance, and intraoperative blood loss. In a study by Forrest et al.,25 pain was presented in 27% of the cases postoperatively which required an average of 5.5 days of parenteral narcotics and analgesics. In our study, one case was presented with persistent pain which continued for 1 month, the pain was moderate in severity and was treated by parenteral anti-inflammatory analgesic for 5 days, after which the pain subsided. Another case presented with gait disturbance due to excessive muscle stripping of iliac muscle intraoperatively, which persisted for more than 2 weeks. The gait disturbance was recorded by assessment of limp deviation, unsteadiness, and unequalness of stride while walking about 20 feet, which were improved by physiotherapy for 2 weeks.26–33
CONCLUSIONS
-
The early repair of orbital floor fracture has a better results and prognosis regarding the objective of treatment.
-
Males were more affected in trauma of orbital floor, with a male to female ratio of 4:1.
-
Enophthalmos was the commonest presentation followed by diplopia, ecchymosis, subconjunctival hemorrhage, limitation of movement, and paresthesia of infraorbital nerve, while epistaxis was the least frequent.
-
Assault trauma was the most frequent cause of injury followed by sport injury, fall from heights, and road traffic accidents. Impure fractures are predominantly caused by high energy trauma, while pure fractures are caused by low energy.
-
Autogenous bone graft procedure is a safe operation for the repair of the orbital floor fractures with less and acceptable postoperative complications as reported in our study and was within the reported proportions of the complications that were reported in literatures and studies.
-
No graft failure or rejection by host was seen in the studied group.
-
The appropriate material for reconstruction of orbital walls is still open for question.
RECOMMENDATIONS
Further studies with larger sample size and longer duration of follow-up are recommended.
To do a comparative study between two or more standardized groups adopting early versus late treatment of orbital floor fractures and compare their outcomes.
Proper early management of traumatic orbital floor fractures with autogenous iliac bone graft will have a good outcome and reduces the adverse sequelae of these injuries.
ETHICAL APPROVAL
The manuscript was written in original, and all the data and results pertaining to this manuscript are original according to the research performed. The authors followed academic integrity and have not copied any content or results from other sources.