BACKGROUND
The novel coronavirus disease (COVID-19) is a global public health emergency. The disease is highly infectious and is characterized mainly by atypical pneumonia, caused by the SARS-CoV-2.1,2 Since the first case of COVID-19 pneumonia was reported in Wuhan, Hubei Province, China, in December 2019, the infection has spread rapidly to the rest of China and beyond. On 12 March 2020, on the basis of more than 20,000 confirmed cases and almost 1000 deaths in Europe, the World Health Organization announced the new coronavirus outbreak as a global pandemic.3 As to the day of writing of this review, more than 5 million confirmed cases and 330,000 deaths due to COVID-19 have been reported.4
No health system was appropriately prepared for the Tsunami-like surge of the COVID-19 pandemic, especially when the number of cases increased exponentially, as in the epicenters of the disease.5 In fact, even hospitals at the forefront have collapsed or ran the risk of collapse when overwhelmed by the exceptionally high number of COVID-19 cases.6 This pandemic had a profound impact on the departments that were responsible for the management of COVID-19 cases, and the consequences have reached almost every specialty in medicine. Almost all nonurgent visits and surgeries were halted in the vast majority of countries with COVID-19 cases.1,7,8 Furthermore, the consequences of the procedures and the steps taken to reduce the spread of infection and to redistribute the resources to deal with this pandemic have not always been appropriately assessed, and remain to be observed. Indeed, some estimates have raised serious concerns regarding the potential devastating consequences as a result of unavoidable shocks, health system collapse, or intentional choices made in response to the pandemic with regard to community morbidity and mortality.1,9
Acquisition of specific new skills may be fundamental in delivering appropriate health care for our patients. The gold standard for the diagnosis of COVID-19 infection is real-time reverse transcription polymerase chain reaction (RT-PCR). Radiological investigations (chest X-ray or high-resolution CT) can be helpful both for diagnosis and management, but they have many limitations. Ultrasound has been suggested as a reliable and accurate tool for assessing the lungs in COVID-19 patients.
COVID-19 AND PREGNANCY
The presence of COVID-19 in a pregnant patient raises concerns, as other types of coronaviruses were frequently associated with an increased risk of adverse outcomes in comparison with the general population of the same age.10–12 Fortunately, to date, there is no evidence that pregnant women are more susceptible to COVID-19 infection, nor to complications and mortality as a result of the disease.13–16 Moreover, there is no evidence of vertical transmission (maternal-to-neonatal) of COVID-19 infection when the maternal infection manifests in the third trimester and of severe adverse outcomes in neonates.17 Another comforting data are the absence of convicing evidence on intrapartum transmission of COVID-19 via vaginal delivery to the neonates.15,17–19 The most common obstetrical complication to COVID-19 seems to be preterm delivery and the high risk of Cesarean delivery.15 Both do not seem to be due to the disease itself, but due to iatrogenic intervention, and more data are needed to understand the relationship between COVID-19 and the mode of delivery and perinatal outcomes.
DIAGNOSIS OF COVID-19
-
The role of clinical assessment: Initially, a history of traveling to areas with a high number of cases, “hot spots,” was often used to define a patient’s risk. Now, in most areas, due to the wide spread of the disease, it is acknowledged that clinical assessment is the main tool to define suspected cases. The most common clinical findings in cases of COVID-19 infection include the following: fever, dry cough, myalgia, fatigue, and dyspnea.20 Less common clinical features are headache, dizziness, abdominal pain, diarrhea, nausea, and vomiting. Common laboratory findings are lymphopenia, prolonged prothrombin time, and elevated lactate dehydrogenase.21 However, a large proportion of cases positive for SARS-CoV-2 will have very mild or no symptoms.22–24 A recent cochrane review concluded that the individual signs and symptoms of COVID-19 appear to have very poor diagnostic properties.25
-
Reverse transcription polymerase chain reaction: The gold standard for COVID-19 infection diagnosis remains the detection of SARS-CoV-2 RNA in nasopharynx samples by RT-PCR.26 Various concerns remain regarding the RT-PCR. These include shortage in kit supplies, especially in low-resource countries. Another major limitation is the rate of false negatives. This may be due to irregular sampling, laboratory error, insufficient viral material in the specimen, improper extraction of nucleic acid from clinical materials, and contamination and technical problems.27,28 The screening policies by RT-PCR and the number of swabs per 1000 citizens remain extremely heterogenous among countries and even regions in the same country.29 COVID-19 is highly contagious; therefore, early detection and diagnosis are of utmost importance to isolate suspected cases to control the outbreak. The above-mentioned challenges in the identification of pathogens by RT-PCR made many clinicians propose radiological investigations as a diagnostic method for identifying COVID-19 patients.30
-
Radiological investigations
-
Computerized tomography
Many studies have demonstrated that CT can be a very useful tool for screening, diagnosis, and follow-up of COVID-19 cases.31 The most frequent CT abnormalities found in patients diagnosed with COVID-19 are ground glass opacity, consolidation, and interlobular septal thickening.32 Lung lesions are usually multiple, and the most involved lung segments are the lower lobes bilaterally. In spite of the several advantages offered by CT, it has some limitations. These include the cost, the high dose of radiation, the need to move the patient across various buildings to be examined by different health personnel, thereby increasing the risk of contamination. In fact, radiology societies have advised against the systematic use of CT and have suggested reducing the number of chest X-rays in COVID-19 patients, to minimize the exposure of health care providers to this viral infection.33 Considering the need to screen and monitor as many patients as possible during the pandemic, lung ultrasound (LUS) was performed with the aim of identifying quickly those patients more likely to be affected by COVID-19.
-
Lung ultrasound
-
Advantages and limitations of LUS (Table 1)
-
Accuracy of LUS in the diagnosis of pneumonia
Many studies have found that LUS is reliable in lung assessment. It has been demonstrated that LUS is sensitive, specific, and reproducible for diagnosing the main lung pathologic entities in patients with Acute Respiratory Distress Syndrome (ARDS). It has thus been advocated that LUS can be considered an attractive alternative to bedside chest X-ray and thoracic computed tomography (CT).44
In addition, LUS seems to be quite reliable in the diagnosis of pneumonia. In a study on patients with community-acquired pneumonia, LUS was found to be helpful in diagnosis with better accuracy in comparison with chest X-ray, using chest CT scan as the gold standard.45 The sensitivity and specificity of LUS was 95 and 90%, respectively. Similar results were found by another multicenter prospective study on patients with various respiratory diseases.46 The authors concluded that LUS should be part of routine diagnostic algorithm of respiratory diseases.
-
Usefulness of LUS in the diagnosis and management of COVID-19
Few data exist on the reliability of LUS in the diagnosis of COVID-19 pneumonia. The diagnostic efficacy seems to depend on the severity of lung involvement, with higher accuracy in more severe cases.47 As this kind of pneumonia is more likely to start from the lateral zone of the lung, close to the pleura, LUS can more effectively demonstrate the pathologic and dynamic changes of the lung condition.48 This characteristic makes LUS an important tool for monitoring the evolution of disease. LUS has high diagnostic accuracy and fewer infection control implications due to decreased patient transportation between various hospital departments. Furthermore, the LUS score provides a degree of objectivity to quantifying the level of involvement, as a comprehensive whole organ assessment.49,50 There is growing evidence suggesting that LUS is accurate both in terms of the diagnosis and the prediction of prognosis and the evolution of lung disease in COVID-19.35,39,40,42,51–54 Indeed, it has been suggested that LUS may be used as a primary imaging modality for pulmonary assessment, thereby reducing the use of chest X-ray in COVID-19 patients.55 LUS can reliably differentiate COVID-19 pneumonia from community-acquired pneumonia.56
-
-
TABLE 1. Advantages and Limitations of LUS
| Advantages | Limitations |
|---|---|
|
|
LUS, lung ultrasound; CT, computerized tomography.
TECHNICAL ASPECTS OF LUS
-
Before you start: safety procedure awareness
When planning an ultrasound examination in the context of the COVID-19 pandemic, some crucial aspects should be considered in addition to the routine procedures. These include mainly:
-
the means to protect the patient and the ultrasound providers.
-
the methods to prepare and clean the ultrasound room and equipment. A recent detailed position statement covering both points has been published by the International Society of Ultrasound in Obstetrics and Gynecology.57
-
-
The transducer
LUS examination can be performed with almost all types of ultrasound machines. Different types of probes can be used: convex, linear, or phased-array.58
-
Machine settings
It is crucial to standardize the machine settings in order to optimize diagnosis and avoid the wrong interpretation of findings in the case of follow-up of the same patients.59
Ultrasound gain should be reduced in order to increase the contrast and highlight the hyperechoic signs. It is recommended to remove contrast enhancement techniques.
-
Patient position
LUS can be performed in supine, sitting, and lateral positions.
-
Lung areas to be examined
Both hemithoraxes should be covered, anteriorly, laterally, and posteriorly, from basal to upper zones. Many approaches have been suggested.60,61
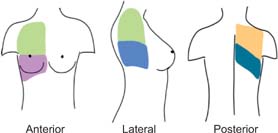
One of the most practical and used approaches can be seen in Figure 1. Each hemithorax is divided into six regions with the aid of anatomical landmarks set by anterior and posterior axillary lines: two anterior, two lateral, and two posterior regions (Figure 2). Each region should be examined in sagittal and axial views.
FIG 1. Areas to be examined using lung ultrasound. Each hemithorax is subdivided into six areas by the anterior and posteior axillary lines.
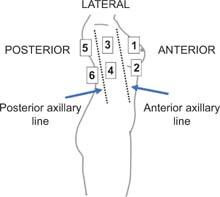
FIG 2. The six regions to be examined by lung ultraound.
NORMAL AND ABNORMAL FINDINGS
-
Normal findings
Pleural line (Figure 3): in a normal lung, only the pleural line can be seen. This appears as a hyperechoic and sliding line, moving forward and backward with ventilation. This is the result of the movement of the visceral pleura against the parietal pleura during the respiratory cycle.
A-lines (Figure 4): these appear as motionless and regularly spaced horizontal lines under the pleural line. These correspond to normal reverberation artefact of the pleural line. A-lines and lung sliding define normal aeration.62
-
Abnormal findings
Abnormal pleural line (Figure 5): in inflammatory lung disease, such as early COVID-19 pneumonia, the pleura line is usually irregular and blurred.39
Well-separated B-lines (Figure 6): one of the hallmarks of acute lung injury is increased extravascular lung water (EVLW), which extends to the lung peripheries. This produces vertical ultrasound artefacts resulting from abnormal gas–tissue interface. B-lines start from the pleural line and “shine” vertically to erase A-lines and reach the end of the screen. The presence of B-lines reflects moderate lung aeration loss resulting from interstitial syndrome. B-lines are often sparse and separated.
Coalescent B-lines (white lung; Figure 7): B-lines may amalgamate, giving the image of “coalescent” B-lines arising from the pleura and spreading to the edge of the screen, denoting more severe lung edema.
FIG 3. Normal pleural line.
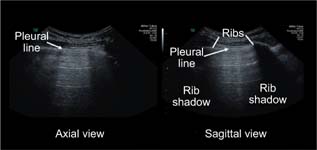
FIG 4. A-lines.
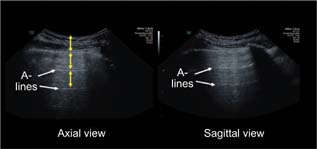
FIG 5. Thickened and irregular pleural line.

FIG 6. B-lines.
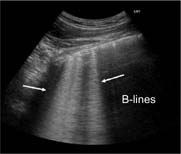
FIG 7. Coalescent B-lines (white lung).

NOTE: “The presence of B-lines denotes interstitial lung disease but does not indicate the pertinent etiology. However, we think that in the context of a COVID-19 pandemic, patients with LUS findings suggestive of interstitial lung disease should be considered to have COVID-19 pneumonia until proven otherwise.”
Lung consolidation (Figure 8): this is due to massive aeration loss. Lungs acquire a tissue-like echotexture (hypoechoic appearance). Lung consolidation usually has a superficial boundary at the level of the pleural line and a deep boundary, which is usually irregular with the aerated lung or regular in the case of whole lobe involvement.
Air bronchogram (Figure 9): sometimes, hyperechoic punctiform images may be seen within the consolidation corresponding to the air-filled bronchi. This is also called air bronchograms. During inspiration, these hyperechoic punctiform images may be reinforced due to penetration of gas into the bronchial tree of the consolidation (the so-called dynamic bronchogram).
FIG 8. Lung consolidation.
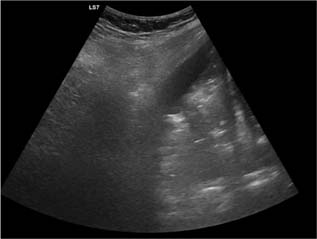
FIG 9. Lung consolidation with air bronchogram.

THE LUNG ULTRASOUND SCORE
Qualitative assessment has been proposed by some authors, while others have suggested the use of a quantitative score.52,62 By attributing each examined region a score per normal or abnormal findings, LUS is the sum of the scores of all examined areas.
Scoring Procedures52: Each examined area is given a score from 0 to 3. Score 0: The pleural line is continuous and regular. Horizontal normal artifacts are present. Score 1: The pleural line is indented, with vertical areas of white lung visible below it. Score 2: The pleural line is broken, with some consolidated areas visible with associated areas of white lung under the breaking point. Score 3: The scanned area shows dense and a largely extended white lung which can also be associated with larger consolidations. At the end of the procedure, the operator will note the highest score obtained for each examined area.
A quantitative score can improve reproducibility. Furthermore, it can be extremely useful in the documentation of the progression or the improvement of lung involvement. Due to its simplicity and the various above-mentioned advantages, some authors tried to examine the accuracy of LUS in screening for COVID-19. It is important to note that while LUS seems accurate and reliable in diagnosing patients with COVID-19 pneumonia, the available data demonstrate that it is unlikely to be a useful screening tool in asymptomatic patients.63–65
LUS IN PREGNANCY
In addition to the already mentioned advantages, LUS has further benefits in pregnant women. Avoiding ionizing radiation is particularly beneficial in pregnancy to prevent fetal exposure. Furthermore, almost all women perform several fetal ultrasound examinations in pregnancy.66
This means that a potential LUS would be practically at zero cost. Various studies on pregnant women showed that LUS is highly accurate in the diagnosis of COVID-19 pneumonia. LUS seems accurate also for the longitudinal monitoring of the pathology in pregnant women and provides a safe and accurate alternative to CT and chest X-ray.43,54,67
To sum up, LUS is a safe, inexpensive, and reliable tool for the assessment of COVID-19. Training various specialists with some experience of ultrasound in other fields seems feasible and efficient, especially in the peak or in preparation for the peak of the COVID-19 outbreak. In spite of its several advantages, it is unlikely that LUS will replace CT in a clinical setting; however, it will probably provide a useful tool in the armamentarium of the clinicians managing COVID-19 patients.
CONCLUSIONS
LUS is a reliable tool for assessing the lungs in COVID-19 patients. LUS can show specific signs of interstitial pneumonia, which is characteristic of COVID-19 pulmonary infection. LUS has many advantages including its relatively rapid learning curve, the bedside applicability, and the absence of ionizing radiation. In pregnancy, LUS can be particularly useful due to the avoidance of the exposure of fetuses to ionizing radiation.