Review Article
Handwashing in averting infectious diseases: Relevance to COVID-19
Mainul Haque
Unit of Pharmacology, Faculty of Medicine and Defence Health, Universiti Pertahanan Nasional Malaysia (National Defence University of Malaysia), Kem Perdana Sungai Besi, Kuala Lumpur, Malaysia
Corresponding author: runurono@gmail.comSubmitted: 6 May 2020. Accepted: 24 June 2020. Published: 12 July 2020.DOI: 10.15586/jptcp.v27SP1.711
ABSTRACT
After officially declared as a pandemic by the World Health Organization (WHO), drastic measures to restrict human movements to contain the COVID-19 infection are employed by most of the countries. Maintaining high personal hygiene by frequent handwashing and be vigilant of clinical signs are widely recommended to reduce the disease burden. The national and international health agencies, including the Centers for Disease Control and Prevention (CDC) and the WHO, have provided guidelines for prevention and treatment suggestions. Here, in this brief article, based on available clinical information, the author discusses why handwashing could be protective of COVID-19 infections. Although a detailed and in-depth discussion of various preventive and protective measures is beyond the scope of this article, this review will focus on the utility of frequent handwashing in minimizing the risk of spreading COVID-19 infection.
Keywords: acute respiratory tract infection, hand hygiene, decontamination, influenza, behavior change, handwashing, hygiene, community, hand sanitizer, influenza infection, influenza transmission, acute gastroenteritis, children, health education, respiratory illness, low- and middle-income countries
INTRODUCTION
Handwashing is an age-old concept. Antoine-Germain Labarraque (March 28, 1777–December 9, 1850), a well-known chemist and pharmacist of France, in the mid-19th century, first revealed that hand cleansing could decrease the occurrence of puerperal infection, fever, and maternal death rates.1 Later in 1847, Hungarian physician, Dr. Ignaz Philipp Semmelweis (July 1, 1818–August 13, 1865), realized that contaminated hand is the major source of transmission of contagious diseases. He introduced and made obligatory for all hospital staff irrespective of the position, including medical students, that all must wash hands with chlorinated lime water before and after examination, resulting in large improvements in death rates.2–6 A meta-analysis reported that good hand hygiene prevents gastrointestinal and respiratory diseases by 31% (95% confidence intervals [CI] = 19%, 42%) and 21% (95% CI = 5%, 34%), respectively.7 This additionally reported prevention of infectious diseases was achieved through non-antimicrobial soap.7 Multiple systematic reviews of handwashing strategies revealed that school absenteeism among school-going children in low- and middle-income (LMICs) and high-income countries (HICs) reduced the incidence of acute respiratory tract infection (ARI), including influenza and pneumonia, and acute gastrointestinal illnesses in community situations.8–12 Although the issue of handwashing remains the same to combat global epidemics, it is important for both HICs and LMICs. Additionally, health professionals and other specialist healthcare stakeholders around the globe facing COVID-19 went through the reality of the current pandemic and advocated that specific methods, line of attack, and interpolations to face the global threat should be community- and country-specific. Hence, three aspects are indispensable: “(1) Reinstatement from countries with ongoing community transmission; (2) the need for extensive testing capacity and widespread community testing, and (3) an adequate supply of personal protective equipment (PPE) to protect healthcare workers.”13 Thereafter, the robust countrywide public health structures based on primary healthcare (PHC) are critical constituents of strong health systems and remain as the first line of combatant against the threat of any pandemic outbreak of diseases as the current COVOD-19. Finally, strong public health competencies and setups need to adopt PHC programs at both community and national levels for effective management of any global public threat.14–16
IMPORTANCE OF HANDWASHING IN INFECTION CONTROL
Hands generally remain dirty and contain pathogenic microbes.17,18 Microbes, generally Enterococcus and Enterobacter spp., possibly from fecal source, were isolated in 44% without hand-washed samples.19 People often touch their eyes, nose, and mouth, but are not aware of harms of such acts. Microbes are transferred from hands to eyes, nose, and mouth, thereby get into the system to develop infectious diseases. Statistics show that handwashing with running water reduces microbial contamination significantly (P < 0.001).19 One meta-regression analysis comprising 42 studies has revealed that handwashing alone minimizes the risk of diarrheal diseases by 40% (risk ratio 0.60; 95% CI 0.53–0.68); however, the adjusted result was 23% (risk ratio 0.77; 95% CI 0.32–1.86).20 Three precautionary health practices, that is to say, wearing face masks, regular handwashing, and home disinfection to improve overall public health status, were widely used during severe acute respiratory syndrome (SARS) in Hong Kong 11.5%–84.3%; 61.5%–95.1%, and 36.4%–80%, respectively. These measures had effectively reduced the risk for transmission (adjusted odds ratio [OR] was 0.58–0.36). These protective hygienic practices were significantly operative in restraining community spread of the SARS respiratory virus.21–23 Another quantitative systematic review regarding respiratory infection comprising 19 “MeSH terms (acute respiratory infections, respiratory disease, respiratory illness, sinusitis, common cold, otitis media, pharyngitis, influenza, coryza, laryngitis, epiglottitis, croup, pneumonia, bronchitis, bronchiolitis, pertussis, and whooping cough)” reported that hand hygiene practice was correlated with lower respiratory microbial transmission and illness. Additionally, hand hygiene practice reduces the risk of acquiring respiratory infection and it ranges from 6–44% (pooled value 24% [95% CI 6–40%]), with a relative risk of 1.19% (95% CI 1.12–1.26%), and the possibility of acquiring respiratory infection with no hand hygiene practice being 16% (95% CI 11–21%).24 Hence, maintenance of proper hand hygiene is considered as a significant preventive strategy for controlling infection in both hospital and community settings.24–28
Finally, “clean care is safer care.”29 World Health Organization (WHO), World Alliance for Patient Safety, and several supervisory, controlling, and endorsing organizations have recommended that hand hygiene is a significant pointer of safety, superiority, and excellence and ensures utmost care provided at any level of healthcare program, because there are considerable data available to establish the correlation between good hand hygiene practices and low healthcare-associated infection (HCAI) rates.30–32
A BRIEF OVERVIEW OF COVID-19
Coronavirus disease 2019 (COVID-19) is a viral infection, instigated by the previously unknown SARS coronavirus-2 (SARS–CoV-2) that was first identified as an epidemic in the city of Wuhan, the capital of Hubei province in China, in December 2019.33,34 COVID-19 is categorized as a respiratory disease resembling influenza with symptoms such as dry cough, fever, exhaustion, ache and pain, sore throat, and shortness of breath. A few affected people have also reported diarrhea, nausea, or a runny nose, and in more severe cases, pneumonia and an acute respiratory syndrome that could lead to death.35,36 This new virus imposes substantial public health catastrophe by causing the SARS, life-threatening pneumonia, and multi-organ dysfunction.25 COVID-19 spreads with a much higher rate than its two progenitors, which are SARS–CoV and Middle East respiratory syndrome coronavirus (MERS–CoV); nonetheless, it possess lower fatality than an earlier family member.37 On March 11, 2020, WHO officially declared COVID-19 a pandemic.38 The pathologic mechanism of COVID-19 is not clear, and therefore the effective intervention strategy could not be developed yet. Despite the advantage of scientific setup and resources, many European countries and the USA are finding it difficult to combat this pandemic, resulting in higher casualties. The healthcare situation of low-resource LMICs is even worse and vulnerable. The archetypal protocol for the management of COVID-19 patients is supportive healthcare as no effective anti-COVID-19 therapy is yet available.39 Consequently, self-protective procedures are the most effective methods to safeguard the community from COVID-19.40 The current focus of healthcare programs in LMICs and HICs to save the lives of COVID-19-infected patients is mostly achieved through different preventive measures.40,41
The current globalization of our planet is rapidly progressing and has consistently changed almost every aspect of human life, interrelated with high international traveling. Hence, health issues, especially infectious disease management, became enormously tricky to control and prevent spread of diseases. Additionally, current COVID-19 pandemic’s biorisk alleviation actions have become a significant challenge for national and international health governing bodies.42–44 Consequently, COVID-19 has become a total global public health catastrophe of the current century and the greatest health challenge that humans have encountered since the Second World War.45 On the other hand, ironically, the global management of COVID-19 pandemic policy planning was not based on public health concerns. Rather, worldwide, political, governmental, national, and international leaders have principally prioritized and depended on mathematical models such as descriptive epidemiology, viral dynamics, and human behavioral factors.46 This research study recommends that no mathematical model alone has the inherent strength to fight a pandemic such as COVID-19.42 At this moment, around the globe, policy makers and government authorities are primarily concentrating on minimizing COVID-19 deaths alone; instead, the focus of policy planning should be on the overall improvement and strengthening of public health status-based PHC for maximizing health and well-being.16,46–48 Moreover, the current policy makers’ healthcare strategy is basically focused on the prevention COVID-19 mortality; hence, almost all health system performances and other health issues have been reduced vividly; subsequently, the mortality rate because of other health conditions has increased intensely.49 The escalation of COVID-19 pandemic in LMICs has brought (or come) to light that enormous differences exist in accessing healthcare within the community and country. However, social and healthcare equity can adequately safeguard millions of marginalized people around the globe.49 Another study has reported that around 55–60% of global population (roughly 4-billion plus people) work in informal sectors without any social security or assistance, and only 20% of people without jobs have jobless welfare assistance.49,50 Hence, this pandemic reminds LMICs that “social protection is, therefore, an indispensable mechanism for delivering support to individuals during the crisis by providing access to healthcare and protecting against the massive losses of income resulting from the deepest economic downturn since the Second World War.”51
IMPACT OF COVID-19 ON HEALTHCARE SYSTEM AND BEYOND
Governments around the globe are implementing the most histrionic intervention policy and planning for the prevention of the current COVID-19 pandemic to save the infected patients.52 Public administrations of almost all countries of the globe are executing multi-level preventive measures from mandatory face masks in public space to total lockdown to stop transmission COVID-19.53–56 Currently, the healthcare system, especially in LMICs, is already stressed to manage both communicable and noncommunicable diseases;57–61 therefore, it is evident that to handle such an enormous public health challenge triggered by the pandemic of COVID-19 will go beyond health and illness.57–62 This pandemic, besides being a human tragedy, has a colossal devastating financial impact on both LMICs and HICs, although it has been reported that the COVID-19 fatalities have skewed to elderly population who are not active working force of the society. Most of the confirmed cases of COVID-19 (86.6%)63 are aged between 30 and 7945 years. The WHO mission revealed that in China, 77.8% of the confirmed cases as on February 20, 2020 were aged between 30 and 69 years.64 Moreover, the principal earning member of the family has lost his/her wages either because of sickness or mortality. In LMICs, the significant workforce comprises daily-based manual laborers; they obtain wages on daily basis, which means no work no pay. Additionally, employers never take any responsibility when their staff is sick or has an accident, even at workplace. Many of these LMICs do not have any old-age retirement benefits. Moreover, many informal sectors do not have paid leave programs and health benefit plans. Consequently, these manual laborers continue to work even if gravely sick, otherwise the whole family will starve. Thus, many experts around the globe think that even if people are saved from COVID-19 pandemic, there would be a high level of morbidities among marginalized communities.65 Again, either public authority or business house impose closure of almost all factories, markets, shops, schools, etc., except essential services such as food and medicine shops, to prevent the community spread of COVID-19 virus, and to protect people. Stay home strategies protect people from the COVID-19 infection, but another truth of life comes in picture, that is, COVID-19 acts as a double edge sword. In this background, it is expected that almost all supply chains will be affected soon because of the COVID-19 lockdown.66 Nevertheless, the most concerning one is the food supply chain interruption. It is described as “the biggest impact that COVID-19 is having on the world’s agricultural system is that of manpower displacement, especially for migrant workers.”67 The major food grain of Asia is rice; usually, its planting season is from the end of April to May. Rice plantation requires a lot of manpower. Typically, the migrant workforce fulfills this need during the plantation season. Additionally, the Asian cultivation process is still dependent on manual labor, not yet mechanized as in the modern world. COVID-19 lockdown crisis has caused human workforce crisis, hence a lot of apprehensions exist for food crisis.67
WAYS HOSPITALS ARE APPLYING INFECTION CONTROL IN RESPONSE TO COVID-19
Following are the key concepts to prevent COVID-19 among healthcare professionals.68
-
Reduce hospital hazards. During the pandemic crisis, all nonessential elective procedures should be deferred, and if possible, telemedicine service should be provided to reduce hospital visits to avoid COVID-19 contacts.
-
Separate infected patients. The suspected or confirmed COVID-19 patients should be isolated to protect patients from hospital-acquired infections and to prevent the spread of this disease.
-
Provide safety to healthcare personnel. Providing adequate number of PPE to healthcare providers and limiting the time of service to avoid overwork and fatigue, which is likely to reduce service.
COVID-19 AND THE CHALLENGES IT POSES FOR LMICS
According to Johns Hopkins University, globally, COVID-19 has infected more than 2.6 million people and at least 183,000 have died till April 22, 2020.69 The challenges of COVID-19 on the healthcare systems are expected to be much different in HICs and LMICs.70 Although LMICs can manage low-order endemic successfully, massive pandemic can quickly produce terrible human misery of this century. Lancet’s editorial describes that the majority of LMICs are not at all ready to face such a catastrophe. LMICs’ healthcare systems are not based on a strong foundation.70 Another recent article describes “the severity of SARS–CoV-2 pneumonia poses a great strain on critical care resources in hospitals, especially if they are not adequately staffed or resourced.”71 Hence, for the last almost five months, statesmen, political leaders, policy makers, and health managers are struggling with the threat of the novel coronavirus pandemic and its worldwide spread.72,73 It was expected that the situation in LMICs would be as worse as possible, with possibly uncountable deaths leading to poverty and disrupting the regional geopolitical environment. Nonetheless, the number of reported cases and mortality rate in South Asia has remained relatively low in comparison to modern countries such as the US, Italy, Spain, France, the UK, etc.74,75 As on April 22, 2020, public authorities of the South Asian Association for Regional Cooperation (SAARC), which comprises India, Pakistan, Bangladesh, Nepal, Sri Lanka, Maldives, Bhutan, and Afghanistan, had reported just 35,297 confirmed cases and 1,021 deaths, despite having a population of 1.7 billion, accounting to 21% of the world’s total population.76,77 COVID-19 deaths (85–90%) principally were among over 60–65-year-old patients.75,78 India, Pakistan and Bangladesh have 5–8% and 2–3% of their populations aged over 60 and 70, respectively.75 in 65 years and above in Italy, France, Spain, UK, and USA 22.752%, 20.035%, 19.375%, 18.396%, and 15.808%, respectively.79 These demographic differences may contribute to the low risk of COVID-19.75 Although India, Pakistan, and Bangladesh have minimal possessions for a social welfare program, the truth is that they have better social bounciness than many HICs. People of these countries commonly do not depend as much on the public system and have higher knowledge, attitude, and practice in managing natural disasters. Moreover, strong community feelings and religious societies could play a valuable role in supporting social resilience.75 Currently, India, Pakistan, and Bangladesh are almost self-reliant for their food production due to high import tax barriers on food imports that make these countries less in need of global food supply chain.75
HAND HYGIENE, COVID-19, AND LMICS
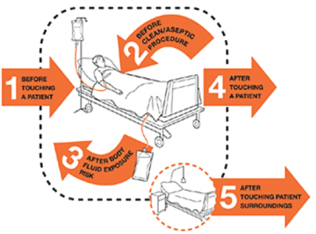
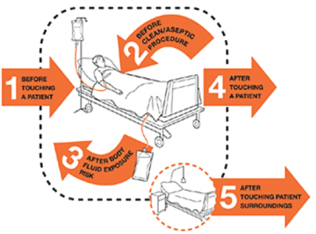
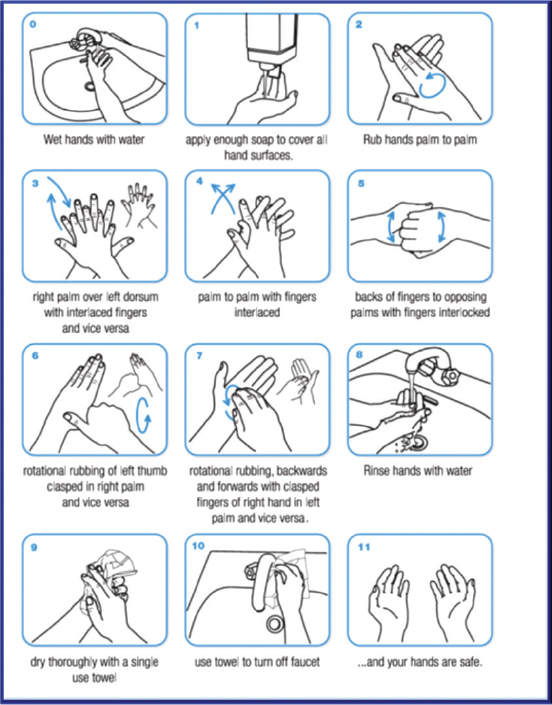
Healthcare-associated infections signify a substantial public health risk to patient safety, distressing patients’ globally by increasing high-level sufferings and death rates, increasing the length of hospital stay, and overall increase in healthcare expenditure for individual as well as community.6,80,81 Hand hygiene practice among healthcare workers (HCWs) is one of the best approaches to minimize the frequency of HCAIs and spread of antimicrobial-resistant microorganisms in both HICs and LMICs, as it is a cheap and effective way to control infection in hospital practice.30,82,83 Moreover, hand hygiene effectively controls pathogenic infection in both patient and healthcare regions.83 The patient sector comprises the patient and his or her immediate settings that include furniture and other inert pieces of stuff that are indicated to be polluted with pathogens of patient. The healthcare sector embraces all other surfaces (including other patients) and possesses high-level contamination by microbes that are external and perhaps contagious to infect the patient.83–85 Thus, the following five approaches of hand hygiene have been advocated: “(1) Before touching a patient. (2) Before clean/aseptic procedures. (3) After body fluid exposure/risk. (4) After touching a patient. (5) After touching patient’s surroundings” (Figure 1). WHO’s strategies and benefits of sanitizing your hands are illustrated in Figures 2 and 3.67,68 Currently, COVID-19 pandemic demands a similar approach to prevent infection, transmission, and safeguarding our community.
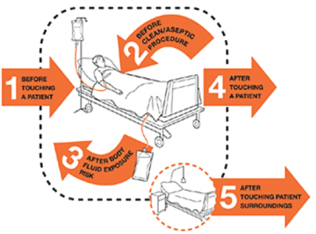
FIG 1. WHO Advocated and Currently Promoting Five Occasions when Health Professionals Must Sanitize their Hands as Essential Requirements for Prevention of COVID-19 Infection.
Source: World Health Organization. WHO guidelines on hand hygiene in healthcare, WHO Press, Geneva, Switzerland, 2009. Available from: https://www.who.int/gpsc/5may/background/5moments/en/ (accessed June 6, 2020).
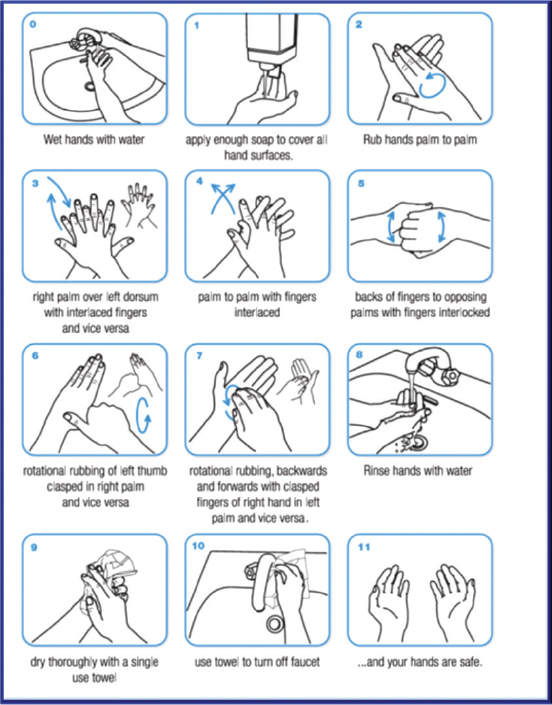
FIG 2. How to Hygienize Your Hands Precisely to Save Yourself from COVID-19 Infection.
Source: United Nations. Handwashing/hand hygiene. Available from: https://www.unwater.org/water-facts/handhygiene/ (accessed June 6, 2020).
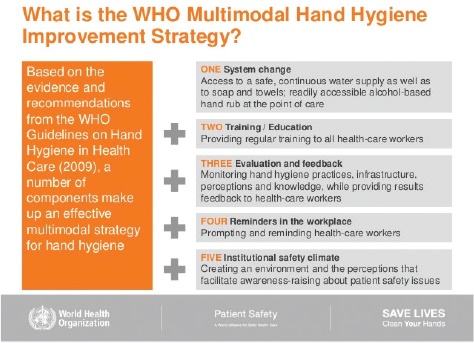
FIG 3. WHO’s Multimodal Hand Hygiene Improvement Strategy in Saving Lives from COVID-19 Global Pandemic.
Source: World Health Organization. WHO Saves Lives: Clean Your Hands, May 5, 2019. “Clean care for all—It’s in your hands.” Available from: https://www.who.int/infection-prevention/campaigns/clean-hands/advocacy-slides-2019_long.pdf?ua=1 (accessed June 6, 2020).
Respiratory infections are usually spread through droplets of diverse sizes86: If the constituent parts of droplets are >5–10 μm in diameter, they are called respiratory droplets, and if they are <5 μm in diameter, they are called droplet nuclei.87–89 Accessing the existing research findings revealed that the COVID-19 virus is mainly communicated among people through respiratory droplets and contact routes.64,90–94 Droplet transmission arises if a person is in close contact, that is within 1 m, of a patient having respiratory disease with coughing, sneezing, etc. and consequently that individual is in danger to have his/her mucosae (mouth and nose) or conjunctiva (eyes) pregnable to those droplets.86 COVID-19 also spreads through objects or materials which are likely to carry infection, such as clothes, utensils, and furniture, in the nearby settings of an infected person. Hence, communication of COVID-19 virus occurs thru (1) direct contact with infected people, and (2) indirect touch with surfaces, floors, door handles, calling bell buzzers, etc. used by the infected person; this can even be possible through physician’s stethoscope or other medical equipment.64,95,96
A study was conducted to compare the following six different handwashing procedures: (1) Soap and water; (2) Alcohol-based hand sanitizer (ABHS); (3) sodium dichloroisocyanurate 0.05% (NaDCC [pH = 6]); (4) high-test hypochlorite (HTH [pH = 11]); (5) high-test hypochlorite stabilized (NaOCl [pH = 11]); and (6) non-stabilized sodium hypochlorite solutions generated (NaOCl [pH = 9–11]) for the prevention of Ebola virus disease (EVD) is reported to be useful.97 A study reported that washing and cleaning contaminated hands with soap and water for 30 s (>3.0 ± 0.4 log10) was statistically significantly efficient than alcohol-based hand sanitizers (2.8 ± 1.5 log10) used in Murine norovirus 1 (MNV1), genomic copies of MNV1 (>5 log10), noroviruses GI.4 (>6 log10), and GII.4 (4 log10). Additionally, propanol-based hand sanitizer demonstrated almost no effect in removing genomic copy of noroviruses GI.4, GII.4, and MNV1 being >2.6, >3.3, and >1.2 log10 polymerase chain reaction (PCR), respectively.98 Soap is principally considered as one of the top cleaning agents for viruses, including COVID-19, for hands because it disintegrates the outer lipid layer of the virus. Soap contains amphiphiles compound, which dissolves the outer lipid layer of COVID-19. Thus, soap and water washing not only removes the COVID-19 virus from hand surface but also kills the life-threatening virus.99,100 Hence, soap and water handwashing and maintaining hand hygiene strategies should be utilized in LMICs to prevent HCAIs and community-acquired infection of COVID-19. However, it is to be mentioned that, in addition to protective handwashing measures, effective antiviral therapeutic agents need to control the severity and progression of the infection. Unfortunately, such specific antiviral therapeutics are yet to be available against COVID-19; till then, handwashing practice is an easy and useful protective measure.
CONCLUSIONS AND RECOMMENDATION
As mentioned, existing evidence shows that frequent handwashing can slow down COVID-19 spread and provides a reasonable health benefits and cost-effective practice to reduce COVID-19-associated disease burden, including respiratory tract infections. In conclusion, maintaining social distancing and practicing simple exercises, such as frequent handwashing, is likely to provide an additional shield against the COVID-19 pandemic, possibly by reducing the hand-to-face viral transmission. In this pandemic situation, frequent handwashing would be a well-intentioned practice. Although in many densely populated LMICs, maintenance of social distancing is a challenging issue because the poverty line is high, people need to live in an extremely crowded environment equally for housing, workplace, and local traveling.40,101,102 Therefore, frequent soap handwashing remains as one of the top preventive measures to the current COVID-19 pandemic—the fatal human health threat of this century.
ACKNOWLEDGMENTS
Thanks to Professor (Dr) MS Razzaque of Lake Erie College of Osteopathic Medicine (USA) for critically reading the manuscript and providing helpful suggestions. The author is much grateful to Professor Judy McKimm of Swansea University, Swansea, Wales, UK, for initial concept-sharing.
CONFLICT OF INTEREST
There are no conflicts of interest.
FINANCIAL SUPPORT AND SPONSORSHIP
This article has not obtained any financial support.
DATA AVAILABILITY STATEMENT
This is review manuscript based on published manuscripts.
COMPLIANCE WITH ETHICAL STANDARDS
This research work based on published manuscripts around the globe. No human or animal experiments involved. Thereby, ethical approval.
REFERENCES
- Labarraque AG. Instructions and Observations Concerning the Use of the Chlorides Soda and Lime. Translated by Porter J. New Haven, CT: Baldwin and Treadway; 1829, 1–42. [Internet]. [cited 2020 July 11]. Available from: https://ia800309.us.archive.org/31/items/62980020R.nlm.nih.gov/62980020R.pdf
- Rotter ML. 150 years of hand disinfection—Semmelweis’ heritage. Hyg Med. 1997;22:332–9. https://doi.org/10.1136/bmj.319.7208.518
- Rotter ML. Semmelweis’ sesquicentennial: A little-noted anniversary of handwashing. Curr Opin Infect Dis. 1998;11(4):457–60. https://doi.org/10.1097/00001432-199808000-00011
- Noakes TD, Borresen J, Hew-Butler T, Lambert MI, Jordaan E. Semmelweis, and the etiology of puerperal sepsis 160 years on a historical review. Epidemiol Infect. 2008;136(1):1–9. https://doi.org/10.1017/S0950268807008746
- Semmelweis I. Classics in Social Medicine. The Etiology, Concept and Prophylaxis of Childbed Fever (Excerpts). Translated by Carter C. 1983. 4–12. The University of Wisconsin Press. [Internet]. [cited 2020 July 11]. Available from: https://www.socialmedicine.info/socialmedicine/index.php/socialmedicine/article/viewFile/178/353
- Haque M, Sartelli M, McKimm J, Abu Bakar M. Healthcare-associated infections—An overview. Infect Drug Resist. 2018;2018(11):2321–33. https://doi.org/10.2147/IDR.S177247
- Aiello AE, Coulborn RM, Perez V, Larson EL. Effect of hand hygiene on infectious disease risk in the community setting: A meta-analysis. Am J Public Health. 2008;98(8):1372–81. https://doi.org/10.2105/AJPH.2007.124610
- McGuinness SL, Barker SF, O’Toole J, et al. Effect of hygiene interventions on acute respiratory infections in childcare, school, and domestic settings in low- and middle-income countries: A systematic review. Trop Med Int Health. 2018;23(8):816–33. https://doi.org/10.1111/tmi.13080
- Wang Z, Lapinski M, Quilliam E, Jaykus LA, Fraser A. The effect of hand-hygiene interventions on infectious disease-associated absenteeism in elementary schools: A systematic literature review. Am J Infect Control. 2017;45(6):682–9. https://doi.org/10.1016/j.ajic.2017.01.018
- Warren-Gash C, Fragaszy E, Hayward AC. Hand hygiene to reduce community transmission of influenza and acute respiratory tract infection: A systematic review. Influenza Other Respir Viruses. 2013;7(5):738–49. https://doi.org/10.1111/irv.12015
- Moncion K, Young K, Tunis M, Rempel S, Stirling R, Zhao L. Effectiveness of hand hygiene practices in preventing influenza virus infection in the community setting: A systematic review. Can Commun Dis Rep. 2019;45(1):12–23. https://doi.org/10.14745/ccdr.v45i01a02
- Mbakaya BC, Lee PH, Lee RL. Hand hygiene intervention strategies to reduce diarrhoea and respiratory infections among schoolchildren in developing countries: A systematic review. Int J Environ Res Public Health. 2017;14(4): 371. https://doi.org/10.3390/ijerph14040371
- Petersen E, Wasserman S, Lee SS, et al. COVID-19—We urgently need to start developing an exit strategy. Int J Infect Dis. 2020;96:233–9. https://doi.org/10.1016/j.ijid.2020.04.035
- Commission on a Global Health Risk Framework for the Future; National Academy of Medicine, Secretariat. The neglected dimension of global security: A framework to counter infectious disease crises, 3, strengthening public health as the foundation of the health system and first line of defense. [Internet]. Washington, DC: National Academies Press (US); 2016. [cited 2020 June 5]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK368392/
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy; Board on Global Health; Committee on Clinical Trials during the 2014-2015 Ebola outbreak. In: Busta ER, Mancher M, Cuff PA, et al., editors. Integrating clinical research into epidemic response: The Ebola experience. Strengthening capacity for response and research [Internet]. Washington, DC: National Academies Press; 2017 [cited 2020 June 05]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441672/
- Haque M, Islam T, Rahman NAA, et al. Strengthening primary health-care services to help prevent and control long-term (chronic) non-communicable diseases in low- and middle-income countries. Risk Manag Healthc Policy. 2020; 2020(13):409–26. https://doi.org/10.2147/RMHP.S241399
- World Health Organization. WHO guidelines on hand hygiene in health care: First global patient safety challenge clean care is safer care. Chapter7. Transmission of pathogens by hands [Internet]. Geneva: World Health Organization; 2009. [cited 2020 June 5]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK144014/
- Burton M, Cobb E, Donachie P, Judah G, Curtis V, Schmidt WP. The effect of handwashing with water or soap on bacterial contamination of hands. Int J Environ Res Public Health. 2011;8(1):97–104. https://doi.org/10.3390/ijerph8010097
- Freeman MC, Stocks ME, Cumming O, et al. Hygiene and health: A systematic review of handwashing practices worldwide and update of health effects. Trop Med Int Health. 2014;19(8):906–16. https://doi.org/10.1111/tmi.12339
- Lau JT, Yang X, Pang E, Tsui HY, Wong E, Wing YK. SARS-related perceptions in Hong Kong. Emerg Infect Dis. 2005;11(3):417–24. https://doi.org/10.3201/eid1103.040675
- Lau JT, Yang X, Tsui H, Kim JH. Monitoring community responses to the SARS epidemic in Hong Kong: From day 10 to day 62. J Epidemiol Community Health. 2003;57(11):864–70. https://doi.org/10.1136/jech.57.11.864
- Lau JT, Tsui H, Lau M, Yang X. SARS transmission, risk factors, and prevention in Hong Kong. Emerg Infect Dis. 2004;10(4):587–92. https://doi.org/10.3201/eid1004.030628
- Tang CS, Wong CY. Factors influencing the wearing of facemasks to prevent severe acute respiratory syndrome among adult Chinese in Hong Kong. Prev Med. 2004;39(6):1187–93. https://doi.org/10.1016/j.ypmed.2004.04.032
- Rabie T, Curtis V. Handwashing and risk of respiratory infections: A quantitative systematic review. Trop Med Int Health. 2006;11(3):258–67. https://doi.org/10.1111/j.1365-3156.2006.01568.x
- Mehta Y, Gupta A, Todi S, et al. Guidelines for prevention of hospital-acquired infections. Indian J Crit Care Med. 2014;18(3):149–63. https://doi.org/10.4103/0972-5229.128705
- Carroll A. Hand washing for health-care workers in domestic care settings. Br J Community Nurs. 2001;6(5):217–23. https://doi.org/10.12968/bjcn.2001.6.5.7081
- Boyce JM, Pittet D; Healthcare Infection Control Practices Advisory Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for hand hygiene in health-care settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep. 2002;51(RR-16):1–CE4.
- Ariza-Heredia EJ, Chemaly RF. Update on infection control practices in cancer hospitals. CA Cancer J Clin. 2018;68(5):340–55. https://doi.org/10.3322/caac.21462
- World Health Organization. World alliance for patient safety. Global patient safety challenge: 2005–2006 [Internet]. World Health Organization, Geneva, 2005 [cited 2020 June 06]. Available from: https://www.who.int/patientsafety/events/05/GPSC_Launch_ENGLISH_FINAL.pdf?ua=1
- Mathur P. Hand hygiene: Back to the basics of infection control. Indian J Med Res. 2011;134(5):611–20. https://doi.org/10.4103/0971-5916.90985
- Pittet D, Allegranzi B, Storr J. The WHO clean care is safer care program: Field-testing to enhance sustainability and spread of hand hygiene improvements. J Infect Public Health. 2008;1(1):4–10. https://doi.org/10.1016/j.jiph.2008.08.006
- Magiorakos AP, Leens E, Drouvot V, et al. Pathways to clean hands: Highlights of successful hand hygiene implementation strategies in Europe. Euro Surveill. 2010;15(18):19560.
- Singhal T. A review of Coronavirus disease-2019 (COVID-19). Indian J Pediatr. 2020;87(4):281–6. https://doi.org/10.1007/s12098-020-03263-6
- Mackenzie JS, Smith DW. COVID-19: A novel zoonotic disease caused by a coronavirus from China: What we know and what we don’t. Microbiol Aust. 2020;41(1):45–50. https://doi.org/10.1071/MA20013
- Harvard Medical School. COVID-19 basics. Symptoms spread and other essential information about the new coronavirus and COVID-19 [Internet]. Harvard Health Publishing 2020 [cited 2020 Apr 22]. Available from: https://www.health.harvard.edu/diseases-and-conditions/covid-19-basics
- National Jewish Health. Coronavirus (COVID-19): Symptoms [Internet]. 2020 [cited 2020 Apr 20]. Available from: https://www.nationaljewish.org/conditions/coronavirus-covid-19/symptoms
- Park SE. Epidemiology, virology, and clinical features of severe acute respiratory syndrome—Coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19). Clin Exp Pediatr. 2020;63(4):119–24. https://doi.org/10.3345/cep.2020.00493
- World Health Organization. WHO director-general’s opening remarks at the media briefing on COVID-19—11 March 2020 [Internet]. WHO 2020 [cited 2020 Apr 22]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42. https://doi.org/10.1001/jama.2020.2648
- Khadka S, Hashmi FK, Usman M. Preventing COVID-19 in low- and middle-income countries. Drugs Ther Perspect. 2020 Apr;13:1–3. https://doi.org/10.1007/s40267-020-00728-8
- Imperial College London. WHO collaborating Centre for Infectious Disease Modelling. The global impact of COVID-19 and strategies for mitigation and suppression [Internet]. MRC Centre for Global Infectious Disease analysis, Abdul Latif Jameel Institute for Disease and Emergency Analytics, Imperial College London; 2020 [cited 2020 Apr 22]. Available from: https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-Global-Impact-26-03-2020v2.pdf
- Bruinen de Bruin Y, Lequarre AS, McCourt J, et al. Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic. Saf Sci. 2020;14(3):104773. https://doi.org/10.1016/j.ssci.2020.104773
- Contini C, Di Nuzzo M, Barp N, et al. The novel zoonotic COVID-19 pandemic: An expected global health concern. J Infect Dev Ctries. 2020;14(3):254–64. https://doi.org/10.3855/jidc.12671
- Institute of Medicine (US) Forum on Microbial Threats. A world in motion: The global movement of people, products, pathogens, and power. In: Knobler S, Mahmoud A, Lemon S, et al., editors. The impact of globalization on infectious disease emergence and control. Exploring the consequences and opportunities: Workshop summary. Proceedings [Internet]. National Academies Press, Washington, DC: 2006 [cited]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK56593/
- Chakraborty I, Maity P. COVID-19 outbreak: Migration, effects on society, global environment, and prevention. Sci Total Environ. 2020;728:138882. https://doi.org/10.1016/j.scitotenv.2020.138882
- Schwalbe N, Hupert N. Models, math, and COVID-19: A public health response [Internet]. International Institute for Global Health, United Nations University; 2020 [cited 2020 June 05]. Available from: https://iigh.unu.edu/publications/articles/models-math-and-covid-19-a-public-health-response.htmlA
- Rothwell DR. Good government, bad government: The politics of public health. US break with WHO: Where does it leave the rest of the world? [Internet]. The Lowy Institute. 2020 [cited 2020 June 05]. Available from: https://www.lowyinstitute.org/the-interpreter/debate/good-government-bad-government-politics-public-health
- Demaio AR, Kragelund Nielsen K, Pinkowski Tersbøl B, Kallestrup P, Meyrowitsch DW. Primary health care: A strategic framework for the prevention and control of chronic non-communicable disease. Glob Health Action. 2014;7(1):24504. https://doi.org/10.3402/gha.v7.24504
- UN News. Workers and COVID-19: Access to healthcare, now ‘a matter of life and death.’ Global perspective Human stories [Internet]. 2020 [cited 2020 June 05]. Available from: https://news.un.org/en/story/2020/05/1064112
- International Labor Organization. Informal economy. More than 60 percent of the world’s employed population are in the informal economy Social protection responses to the COVID-19 pandemic in developing countries: Strengthening resilience by building universal social protection [Internet]. Social Protection Spotlight. 2018 [cited 2020 June 05]. Available from: https://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_627189/lang--en/index.html
- International Labor Organization. Social protection responses to the COVID-19 pandemic in developing countries: Strengthening resilience by building universal social protection [Internet]. Social Protection Spotlight. 2020 [cited 2020 June 05]. Available from: https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---soc_sec/documents/publication/wcms_744612.pdf
- Pell MB, Lesser B. The COVID-19 lockdown will take its own toll on health, researchers warn [Internet]. World Economic Forum. 2020 [cited 2020 Apr 22]. Available from: https://www.weforum.org/agenda/2020/04/how-the-covid-19-lockdown-will-take-its-own-toll-on-health/
- Nortajuddin A. COVID-19: Debunking myths [Internet]. The ASEAN Post. [cited 2020 Apr 22]. Available from: https://theaseanpost.com/article/covid-19-debunking-myths
- Financial Times. Coronavirus: Trump orders the US to halt funding to WHO—as it happened [Internet]. 2020 [cited 2020 Apr 22]. Available from: https://www.ft.com/content/59ff62ae-3f66-3ec2-b269-e94e9a72f198
- Yulisman L. Coronavirus pandemic. Compulsory for Indonesians to wear masks in public [Internet]. The Straits Times. 2020 [cited 2020 Apr 22]. Available from: https://www.straitstimes.com/asia/se-asia/compulsory-for-indonesians-to-wear-masks-in-public
- The Guardian. How far? How soon? Czechs grapple with how to ease COVID-19 lockdown [Internet]. 2020 [cited 2020 Apr 22]. Available from: https://www.theguardian.com/world/2020/apr/19/czechs-grapple-with-how-to-ease-covid-19-lockdown
- Islam SM, Purnat TD, Phuong NT, Mwingira U, Schacht K, Fröschl G. Non-communicable diseases (NCDs) in developing countries: A symposium report. Global Health. 2014;10(81):81. https://doi.org/10.1186/s12992-014-0081-9
- Rule J, Ngo DA, Oanh TT, et al. Strengthening primary health care in low- and middle-income countries: Generating evidence through evaluation. Asia Pac J Public Health. 2014;26(4):339–48. https://doi.org/10.1177/1010539513503869
- Kruk ME, Nigenda G, Knaul FM. Redesigning primary care to tackle the global epidemic of noncommunicable disease. Am J Public Health. 2015;105(3):431–7. https://doi.org/10.2105/AJPH.2014.302392
- Bardossy AC, Zervos J, Zervos M. Preventing hospital-acquired infections in low-income and middle-income countries: Impact, gaps, and opportunities. Infect Dis Clin North Am. 2016;30(3):805–18. https://doi.org/10.1016/j.idc.2016.04.006
- Palagyi A, Marais BJ, Abimbola S, Topp SM, McBryde ES, Negin J. Health system preparedness for emerging infectious diseases: A synthesis of the literature. Glob Public Health. 2019;14(12):1847–68. https://doi.org/10.1080/17441692.2019.1614645
- Alessi C.The effect of the COVID-19 epidemic on health and care—Is this a portent of the ‘new normal’? [Internet]. Healthcare IT News. Europe/UK. Population Health. 2020 [cited 2020 Apr 22]. Available from: https://www.healthcareitnews.com/blog/europe/effect-covid-19-epidemic-health-and-care-portent-new-normal
- The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020[J]. China CDC Weekly. 2020;2(8):113–22.
- World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19) [Internet]. 2020 [cited 2020 Apr 22]. Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
- Evans D, Over M. The economic impact of COVID-19 in low- and middle-income countries [Internet]. Center for Global Development; 2020 [cited 2020 Apr 22]. Available from: https://www.cgdev.org/blog/economic-impact-covid-19-low-and-middle-income-countries
- Mckenzie B. Beyond COVID-19: Supply chain resilience holds the key to recovery [Internet]. Oxford Economics; 2020 [cited 2020 Apr 22]. Available from: https://www.bakermckenzie.com/-/media/files/insight/publications/2020/04/covid19-global-economy.pdf
- Neo P. COVID-19’s crop crisis: Pandemic poses a major risk to Asia’s food supply and trade—Expert [Internet]. 2020 [cited 2020 Apr 22]. Available from: https://www.foodnavigator-asia.com/Article/2020/04/15/COVID-19-s-crop-crisis-Pandemic-poses-major-risk-to-Asia-s-food-supply-and-trade-expert?utm_source=copyright&utm_medium=OnSite&utm_campaign=copyright
- Centers for Disease Control and Prevention. Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings [Internet]. National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases. 2020 [cited 2020 Apr 23]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
- Westcott B, Renton A. Live updates. Coronavirus pandemic: Updates from around the world [Internet]. 2020 [cited 2020 Apr 23]. Available from: https://edition.cnn.com/world/live-news/coronavirus-pandemic-04-23-20-intl/index.html
- The Lancet. COVID-19: Too little, too late? Lancet. 2020;395(10226):755. https://doi.org/10.1016/S0140-6736(20)30522-5
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–81. https://doi.org/10.1016/S2213-2600(20)30079-5
- Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–3. https://doi.org/10.1016/S0140-6736(20)30185-9
- Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33. https://doi.org/10.1056/NEJMoa2001017
- Bhutta ZA, Basnyat B, Saha S, Laxminarayan R. COVID-19 risks and response in South Asia. BMJ. 2020;368:m1190. https://doi.org/10.1136/bmj.m1190
- Brewster D. Why South Asia may come out of the COVID-19 crisis better than many expect [Internet]. 2020 [cited 2020 Apr 24]. Available from: https://www.lowyinstitute.org/the-interpreter/why-south-asia-may-come-out-covid-19-crisis-better-many-expect
- Sajid I. South Asia: Virus cases top 35,000, deaths pass 1,000 India is region’s hardest-hit country, followed by Pakistan, Bangladesh, and Afghanistan [Internet]. [cited 2020 Apr 24]. Available from: https://www.aa.com.tr/en/asia-pacific/south-asia-virus-cases-top-35-000-deaths-pass-1-000/1814760#
- World Population Review. SAARC countries, 2020 [Internet]. 2020 [cited 2020 Apr 24]. Available from: https://worldpopulationreview.com/countries/saarc-countries/
- European Center for Disease Prevention and Control. Coronavirus disease 2019 (COVID-19) in the EU/EEA and the UK—Eighth update. Rapid Risk Assessment [Internet]. 2020 [cited 2020 Apr 24]. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-rapid-risk-assessment-coronavirus-disease-2019-eighth-update-8-april-2020.pdf
- The World Bank. Population ages 65 and above (% of the total population) [Internet]. 2019 [cited 2020 Apr 24]. Available from: https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?locations=US-IT-FR-ES-GB
- Collins AS. Preventing health care-associated infections. In: Hughes RG, editor. Patient safety and quality: An evidence-based handbook for nurses. Chapter 41 [Internet]. Rockville, MD: Agency for Healthcare Research and Quality (US); 2008 [cited 2020 Apr 24]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2683/
- Zhou Q, Fan L, Lai X, Tan L, Zhang X. Estimating extra length of stay and risk factors of mortality attributable to healthcare-associated infection at a Chinese university hospital: A multi-state model. BMC Infect Dis. 2019;19(1):975. https://doi.org/10.1186/s12879-019-4474-5
- Anargh V, Singh H, Kulkarni A, Kotwal A, Mahen A. Hand hygiene practices among healthcare workers (HCWs) in a tertiary care facility in Pune. Med J Armed Forces India. 2013;69(1):54–6. https://doi.org/10.1016/j.mjafi.2012.08.011
- Loftus MJ, Guitart C, Tartari E, et al. Hand hygiene in low- and middle-income countries. Int J Infect Dis. 2019;86:25–30. https://doi.org/10.1016/j.ijid.2019.06.002
- Sax H, Allegranzi B, Chraïti MN, Boyce J, Larson E, Pittet D. The World Health Organization hand hygiene observation method. Am J Infect Control. 2009;37(10):827–34. https://doi.org/10.1016/j.ajic.2009.07.003
- Sax H, Allegranzi B, Uçkay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene’: A user-centered design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67(1):9–21. https://doi.org/10.1016/j.jhin.2007.06.004
- Atkinson J, Chartier Y, Pessoa-Silva CL, et al., editors. Natural ventilation for infection control in health-care settings. Annex C, Respiratory droplets [Internet]. Geneva: World Health Organization; 2009 [cited 2020 Apr 24]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK143281/
- Tellier R, Li Y, Cowling BJ, Tang JW. Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect Dis. 2019;19(1):101. https://doi.org/10.1186/s12879-019-3707-y
- Kucharski AJ, Russell TW, Diamond C, et al. Early dynamics of transmission and control of COVID-19: A mathematical modeling study. Lancet Infect Dis. 2020;20:553–58. https://doi.org/10.1016/S1473-3099(20)30144-4
- Wu JT, Leung K, Bushman M, et al. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat Med. 2020;26(4):506–10. https://doi.org/10.1038/s41591-020-0822-7
- Liu J, Liao X, Qian S, et al. Community Transmission of Severe Acute Respiratory Syndrome Coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis. 2020;26(6):1320–1323. https://doi.org/10.3201/eid2606.200239
- Chan J, Yuan S, Kok K, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet. 2020;395:514–23. https://doi.org/10.1016/S0140-6736(20)30154-9
- Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–207. https://doi.org/10.1056/NEJMoa2001316.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
- Burke RM, Midgley CM, Dratch A, et al. Active monitoring of persons exposed to patients with confirmed COVID-19—United States, January–February 2020. MMWR Morb Mortal Wkly Rep. 2020;69(9):245–6. https://doi.org/10.15585/mmwr.mm6909e1external icon
- Marinella MA. COVID-19 pandemic and the stethoscope: Don’t forget to sanitize. Heart Lung. 2020;49:350. https://doi.org/10.1016/j.hrtlng.2020.03.017
- World Health Organization. Modes of transmission of the virus causing COVID-19: Implications for IPC precaution recommendations [Internet]. 2020 [cited 2020 Apr 24]. Available from: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations
- Wolfe MK, Gallandat K, Daniels K, Desmarais AM, Scheinman P, Lantagne D. Handwashing and Ebola virus disease outbreaks: A randomized comparison of soap, hand sanitizer, and 0.05% chlorine solutions on the inactivation and removal of model organisms Phi6 and E. coli from hands and persistence in rinse water. PLoS One. 2017;12(2):e0172734. https://doi.org/10.1371/journal.pone.0172734
- Tuladhar E, Hazeleger WC, Koopmans M, Zwietering MH, Duizer E, Beumer RR. Reducing viral contamination from finger pads: Handwashing is more effective than alcohol-based hand disinfectants. J Hosp Infect. 2015;90(3):226–34. https://doi.org/10.1016/j.jhin.2015.02.019
- Thordarson P. The science of soap—Here’s how it kills the coronavirus [Internet]. The Guardian. 2020 [cited 2020 Apr 24]. Available from: https://www.theguardian.com/commentisfree/2020/mar/12/science-soap-kills-coronavirus-alcohol-based-disinfectants
- Centers for Disease Control and Prevention. Cleaning and disinfection for households. Interim recommendations for U.S. households with suspected or confirmed coronavirus disease 2019 (COVID-19) [Internet]. CDC 2020 [cited 2020 Apr 24]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cleaning-disinfection.html
- Jha A, Kawoosa VM. Why social distancing is tough to implement. The first problem in implementing social distancing in India could be its population density itself [Internet]. Hindustan Times. 2020 [cited 2020 June 6]. Available from: https://www.hindustantimes.com/india-news/why-social-distancing-is-tough-to-implement/story-iTp2VbV2GQxEvIeSwoOMCK.html
- Hopman J, Allegranzi B, Mehtar S. Managing COVID-19 in low- and middle-income countries. JAMA. 2020;323(16):1549–50. https://doi.org/10.1001/jama.2020.4169