Pictorial Essay
Cerebral abscesses imaging: A practical approach
Paola Feraco,1,2 Davide Donner,3 Cesare Gagliardo,4 Irene Leonardi,1 Silvia Piccinini,5 Anna del Poggio,6 Rossana Franciosi,7 Benedetto Petralia1 and Luc van den Hauwe8
1Department of Neuroradiology, Ospedale S. Chiara, Azienda Provinciale per i Servizi Sanitari, Trento, Italy
2Department of Experimental, Diagnostic and Specialty Medicine (DIMES), University of Bologna, Bologna, Italy
3Department of Nuclear Medicine, S. Chiara Hospital, Azienda Provinciale per i Servizi Sanitari, Trento, Italy
4Section of Radiological Sciences, Department of Biomedicine, Neurosciences and Advanced Diagnostics, University of Palermo, Palermo, Italy
5Neuroradiology Unit, Ospedale Civile S. Agostino-Estense University Hospital, Modena, Italy
6Neuroradiology Department, San Raffaele Scientific Institute, Milan, Italy
7Radiology Unit, S. Maria del Carmine Hospital, Rovereto, Italy
8Department of Radiology, University of Antwerp, Antwerp, Belgium
Corresponding author: paola.feraco@apss.tn.itSubmitted: 28 April 2020. Accepted: 29 May 2020. Published: 11 July 2020.DOI: 10.15586/jptcp.v27i3.688
ABSTRACT
Brain abscesses (BAs) are focal infections of the central nervous system (CNS) that start as a localised area of weakening of the brain parenchyma (cerebritis) and develops into a collection of pus surrounded by a capsule.
Pyogenic (bacterial) BAs represent the majority of all BAs; in some cases, the diagnostic and therapeutic management can be challenging. Imaging has a primary role in differentiating BAs from other lesions. Conventional magnetic resonance imaging (cMRI) is essential for the identification of the lesion, its localisation and its morphological features. However, cMRI does not allow to reliably differentiate BAs from other intracranial mass lesions such as necrotic tumours. Advanced sequences, such as diffusion-weighted imaging (DWI), perfusion-weighted imaging (PWI) and proton MR spectroscopy (1H-MRS) are very useful in the differential diagnosis from other brain lesions, such as non-pyogenic abscesses or necrotic tumours, and provide essential information on structural, vascular and metabolic characteristics allowing greater neuroradiological confidence. The aim of this pictorial review is to provide a practical approach showing the added value of more advanced MRI techniques in their diagnostic management.
Keywords: brain abscess, magnetic resonance imaging (MRI), diffusion weighted imaging (DWI), magnetic resonance spectroscopy (MRS)
INTRODUCTION
Brain abscesses (BA) are focal infections of the central nervous system (CNS). They account for 1–2% of brain occupying space lesions in western countries and 8% in developing countries.1 Main predisposing conditions are contiguous spread of pathogens (50% of the cases) following otitis or mastoiditis, sinusitis, meningitis, neurosurgery or traumatic brain injury or through haematogenous dissemination. However, the primary site of infection remains unknown in 40% of cases.2 According to the site of the BA, symptoms may be different; these include in decreasing order: headache, fever, focal neurologic deficit, seizures and mental status changes. Consequently, the diagnostic and therapeutic management can be challenging. Imaging has a primary role in differentiating BA from other lesions using MR as the technique of choice for diagnosis and follow-up. The aim of this pictorial review is to provide a practical approach, showing the added value of advanced MRI techniques, such as diffusion-weighted imaging (DWI), perfusion-weighted imaging (PWI) and proton MR spectroscopy (1H-MRS), in their diagnostic management.
Aetiology and Pathogenesis
Bacteria are responsible for more than 95% of BA in immunocompetent patients. The brain is particularly vulnerable to bacterial infections once the blood–brain barrier has been crossed. The bacterial species depend on the primary site of infection and are summarised in Table 1. The most frequent occurrence of a pyogenic BA is the supratentorial region, in the subcortical white matter. BA secondary to middle ear otitis are usually located in the temporal lobe or in the cerebellum, while a localisation of a pyogenic abscess in the basal ganglia is rare.3 Although the BA is usually an isolated lesion in immunocompromised patients it is frequent to find multiple lesions. The typical pyogenic BA is formed by a central necrotic tissue surrounded by an external wall that is composed of collagen, granulation tissue, macrophages and gliosis.4 The early parenchymal infection starts as a cerebritis and then progresses through four stages to form an abscess.
TABLE 1. Bacterial Aetiologies Related to the Primary Site of Infection
| Way of Infection |
Particular Categories of Patient |
| Neurosurgical Procedures |
ENT Surgery |
Haematogenus Dissemination |
Dental Infection |
Immunocompromised Patients |
S. aureus, S. epidermidis,
Clostridium, Actinomyces |
Streptococcus species;
Staphylococcus species. |
S. aureus, Streptococcus species, Bacteria from HACE K group
(Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, Kingella) |
Polymicrobial, (often with anaerobic bacteria like Bacteroides, Fusobacterium, Actinomyces); |
Frequent:
Mycobacterium tuberculosis or Mycobacterium avium complex
Infrequent:
Nocardia species; L. monocytogenes, Rhodococcus equi; |
- early cerebritis (1st to 3rd day—characterised by an inflammatory response);
- late cerebritis (4th to the 9th day—central necrosis formation, peripheral angiogenesis and presence of fibroblasts);
- early encapsulation (10th to the 13th day—surrounding peripheral wall with the persistence of central necrosis);
- late capsule stage (14th day and forward—mature encapsulate BA with a wide central necrotic area);
It is not frequent to find the presence of air in the abscess and it may be associated with Clostridium, Klebsiella, Enterobacter or Pseudomonas.5
Astrogliosis and cerebral oedema are seen surrounding the abscess capsule. Gliosis can persist after treatment, and constitutes a major risk factor for the development of post-infective epilepsy.6
IMAGING FEATURES
Pyogenic Abscesses
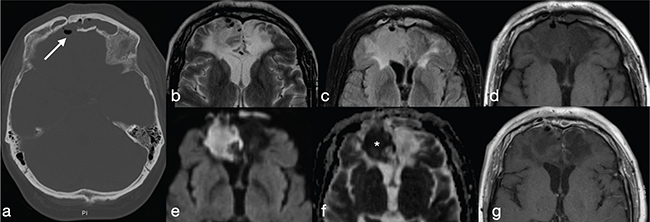
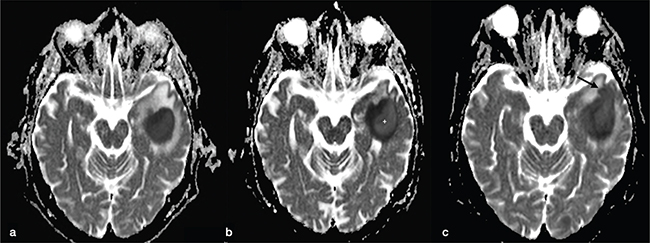
Early cerebritis is seen as a nonspecific focus of oedema with or without contrast enhancement. It appears as an ill-defined area, hypointense on T1-weighted images (wi) and hyperintense on FLAIR and T2-wi. Using DWI may help to differentiate cerebritis from other lesions as it shows restricted diffusion (i.e., low signal in apparent diffusion coefficient-ADC) (Figure 1). Mature pyogenic BAs usually are round or oval-shaped with a central cavity filled with pus, hypointense on T1-wi and hyperintense on T2-wi.
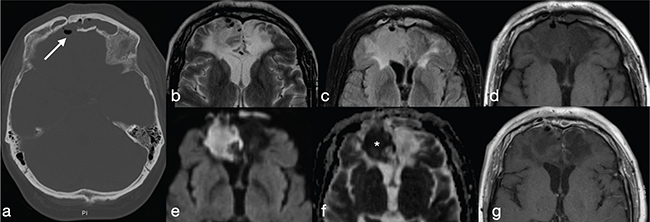
FIG 1. Early Cerebritis in a 57-Year-Old Man who Presented with Headache, Fever and Lethargy after a Previous History of Motorcycle Accident. (a) Brain CT shows post-traumatic sequelae in the basifrontal areas with a defect in the posterior wall of the right frontal sinus and associated pneumocephalus (arrow); within the wider ill-defined area of parenchymal contusion (b–d, g), an area of restricted diffusion (e–f) with no contrast-enhancement (g) consistent with early cerebritis, is shown.
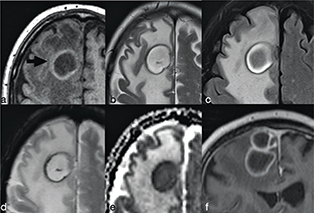
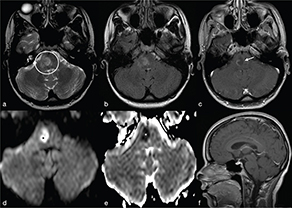
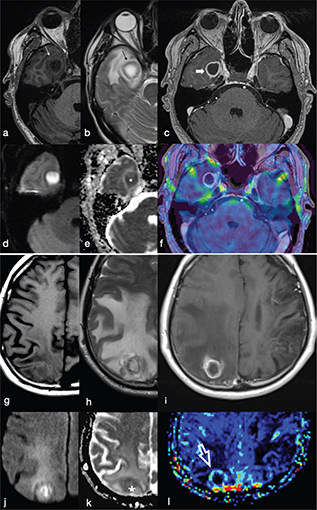
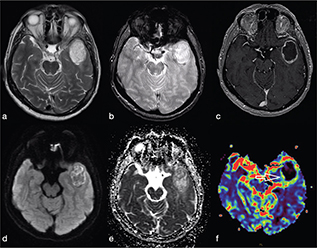
The abscess capsule is well-defined, smooth and complete. It shows a layered aspect, hypointense on FLAIR/T2-wi and hyperintense on T1-wi. The presence of collagen fibres and macrophages releasing free radicals are considered responsible for the short T1 and T2 of the rim due to their paramagnetic effect (Figure 2).7 The external low-signal rims on T2-wi could be useful to distinguish abscess from glioblastomas: in this case the rims, irregular or incomplete in the majority of cases, result from the store of haemorrhagic products surrounding the outer layer of the necrotic core.8
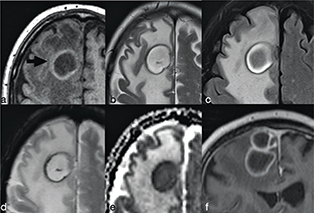
FIG 2. Nocardia Abscess in a 64-Year-Old Immunocompromised Man Presenting with Headache. A round lesion with thick capsule hyperintense on T1w (a) and hypointense on T2w/FLAIR-T2w (b–c) is shown. The lesion is characterised by a core of restricted diffusion (d–e). Typical ring-enhancement is present after intra-venous Gd administration; the coronal scan also reveals the presence of multiple lesions (f). A discreet amount of perilesional vasogenic oedema is present too (a–e).
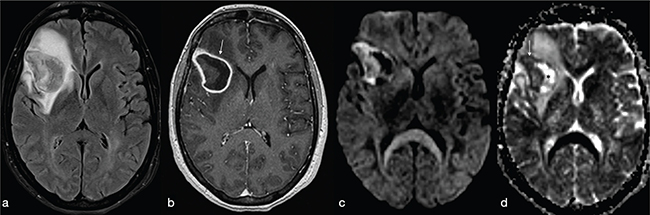
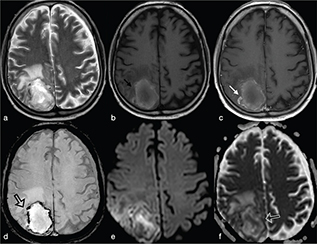
On FLAIR/T2-wi, the abscess is usually surrounded by vasogenic oedema. Moreover, FLAIR images can be useful to help improve the diagnosis of a subarachnoid rupture of the BA with subsequent meningitis (Figure 3). Satellite abscesses that give a polylobate appearance to the BA can occur (Figure 4).
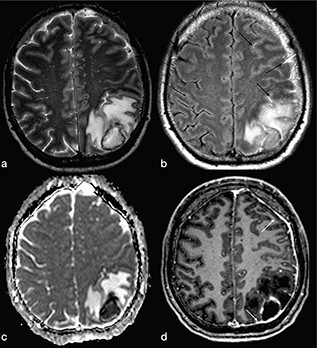
FIG 3. A 45-Year-Old Man with Pyogenic Abscess Surfacing the Left Parietal Lobe Cortex. A roundish mass with a core of necrotic-cystic degeneration (a–b) showing restricted diffusion on ADC maps (c) and diffuse surrounding vasogenic oedema (a–c) with irregular rim-enhancement (d) is shown. FLAIR-T2w (b) high signal within the subarachnoid spaces reveals rupture of abscess into the subarachnoid space (black arrows in b). Meningeal involvement is also appreciable after i.v. administration of Gd (white arrows in d).
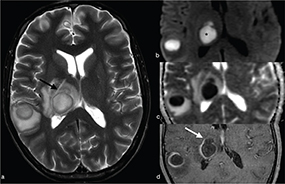
FIG 4. A 54-Year-Old Woman with Multiple Pyogenic Abscesses Involving the Right Thalamus and Right Temporal Region. The abscesses show a thin capsule on T2w (a) binding a core of restricted diffusion (asterisk in b) with correspnding low signal in ADC maps (c). Smooth ring enhancement on gadolinium-enhanced T1w (d) is present. Satellite abscesses (black and white arrows in a and d respectively) give a polylobulated appearance.
After intravenous injection of gadolinium (Gd), a variable degree of contrast-enhancement of the capsule can be detected (Figure 5), depending on the evolutional stage of the abscess.7 A well-defined ring-enhancement can be detected only in the late evolutive stage of the BA. Due to the higher vascularity, the peripheral enhancement of BAs is thicker along the outer margin compared to the inner margin (Figure 6).9
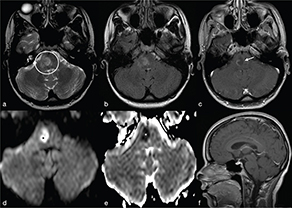
FIG 5. A 20-Year-Old Woman with Early Listeria Monocytogenes Rhombencephalitis who Presented with Progressive Left-Sided Sensory Deficits and Left Hemiparesis. On T2w (a) and FLAIR-T2w (b) a focal ill-defined area of high signal intensity in the right hemipons (open circle in a) is observed. T1w+Gd shows a peripheral irregular enhancement (c, f) while the lesional core is a clear restriction of water molecules diffusion (asterisks in d-e).
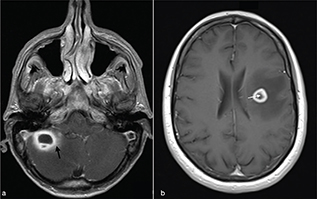
FIG 6. Pattern of Ring Enhancement in Actinomyces Abscess (a) and Glioblastoma (GBM) (b). Complete and smooth ring enhancement on gadolinium-enhanced T1w is present in both lesions. The abscess usually shows a thicker peripheral enhancement along the outer margin compared with GBM (arrows).
On susceptibility-weighted imaging (SWI) pyogenic BAs show a typical hyperintense inner layer and hypointense outer layer surrounding the central cavity, called the “dual rim” sign (Figure 7).10 Indeed, due to granulation tissue of the capsule, SWI sequence can be appropriate to help differentiate pyogenic BA from other ring-enhancing lesions such as necrotic tumour, fungal abscesses and demyelinating lesions (see later).
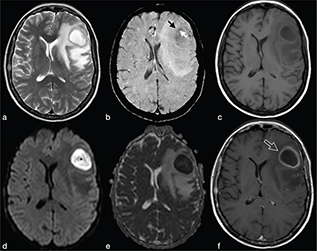
FIG 7. A 37-Year-Old Woman with Pyogenic Abscess in the Left Frontal Lobe. The capsule of the abscess, hypointense on T2w (a) and slight hyperintense on T1w (c), and shows the typical “dual rim sign” on SWI (b): low signal of the external rim (black arrow) and high signal of the inner layer (white arrow). The central component of the lesion shows high signal in DWI (asterisk in d) and low signal in the ADC maps (e) consistent with restricted diffusion. (f) Contrast media administration reveals a thick regular ring enhancement (f).
Advanced MRI and PET Techniques
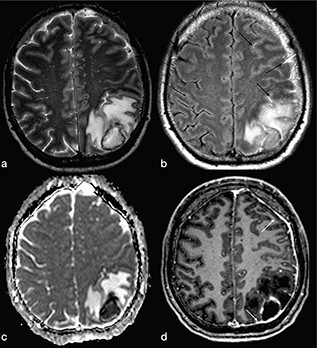
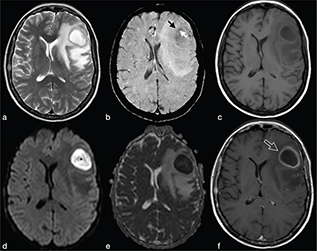
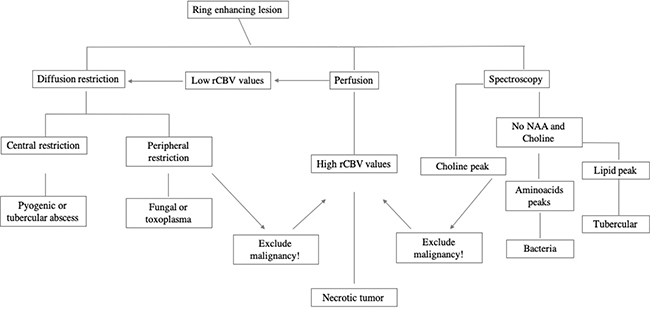
Pyogenic BAs are typically hyperintense on DWI, with low ADC values. This finding is due to the restricted motion of water in the BA cavity that contains pus: inflammatory cells, bacteria, necrotic tissue and a proteinaceous exudate with a very high viscosity and cellularity (Figure 4 and Figures 7-9).11 ADC values may have a wide range due to the different compositions of the abscess cavity, the different types of bacteria involved and the immune response of the host.12,13 Changes in ADC values on post-treatment follow-up MRI may be observed. Increasing ADC values in the abscess cavity are an early indicator of successful treatment (Figure 10). These changes in ADC values can be observed before the size reduction of the BA.12 Conversely, persistently low ADC values could represent an ineffective drug therapy, and recurrence of low ADC values might suggest active disease (Figure 9).14 DWI is also useful in improving the diagnosis of an intraventricular rupture of the BA with subsequent ventriculitis.
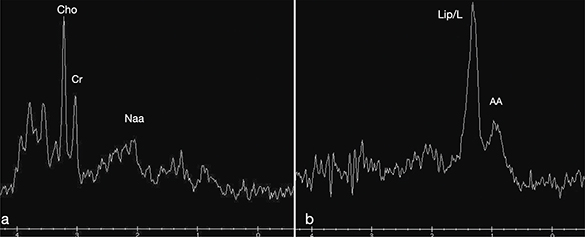
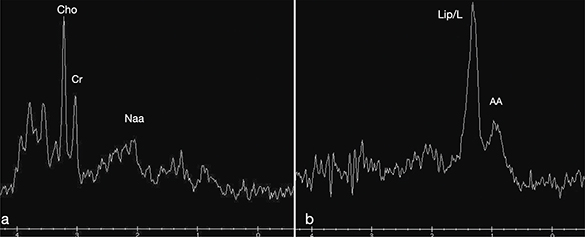
FIG 8. 1H-MRS Spectra in a Glioblastoma (a) and a Brain Abscess (b). The resonance peaks from the tumour typically represent a high choline (Cho) peak and low creatine (Cr) and N-acetyl-aspartate (NAA) peaks. The abscess cavity shows resonance peaks representing cytosolic amino acids (AA, 0.9 ppm), lipids/lactate (Lip/L, peak-doublet centred at 1.33 ppm) without Cr, Cho and NAA peaks.
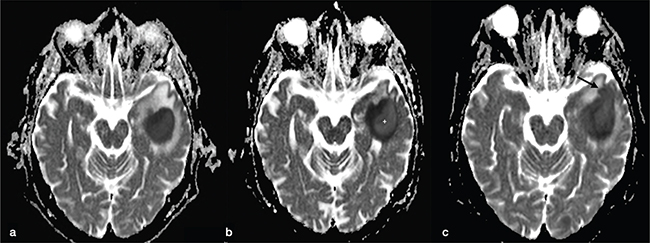
FIG 9. Longitudinal Follow-Up MRI Studies of a Pyogenic Abscess in a 54-Year-Old Alcoholic Man Admitted to the ER with Epileptic Seizures. Blood cultures were positive for methicillin-sensitive Staphylococcus aureus. (a) On the first brain MRI, the left temporal lesion showed marked restricted diffusion with low signal intensity on the ADC map, typical for a pyogenic abscess. (b) After 2 weeks of antibiotic therapy (oxacillin: 2 g six times a day) a new MRI was performed. No change in lesion size was observed but increased signal in the central-lateral portion of the core of the abscess on the ADC map was noticed (asterisk) suggestive of good therapy response. (c) Unfortunately, follow-up MRI performed after two more weeks of antibiotic therapy revealed signs of disease progression with an increase in size, satellite lesion (arrow in c), almost unchanged ADC values and more perilesional vasogenic oedema.
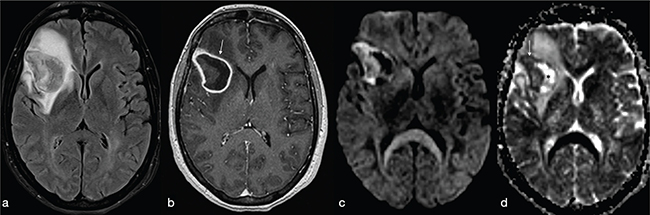
FIG 10. Follow-Up Exam of a Pyogenic Brain Abscess (Streptococcus pneumoniae) in a 62-Year-Old Woman who Presented with Headaches and Behavioural Disorders. (a) The right frontal lesion is surrounded by vasogenic oedema and the signal intensity of the lesional core is partially suppressed on FLAIR-T2w (a) because of its proteinaceous content. Intravenous administration of contrast reveals a typical ring enhancement (arrow in b). The abscess core reveals a variable signal intensity on both DWI sequences (c) and ADC map (asterisk and arrow in d) related to a favourable therapy response.
PWI provides information about the vascularisation of a lesion. Usually, PWI in pyogenic BA demonstrate low relative cerebral blood volume (rCBV) in the capsule, whereas necrotic brain tumours show elevated rCBV as a result of neoangiogenesis within the tumour tissue (Figure 11).11 This technique may be useful in the differential diagnosis of ring-like enhancing brain lesions that may mimic BA. These include neoplastic lesions (glioblastoma, metastases) and demyelinating lesions. However, rCBV values may vary according to the stage of the capsule: higher in the early stage than in the late stage in which the fibroblasts are dominant.5,11
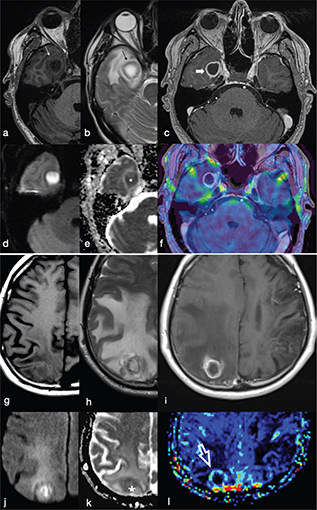
FIG 11. Differences between a Pyogenic Brain Abscess (a-f) and a Hypercellular Lung Metastasis (g-l). The peripheral ring of the abscess and cystic metastasis are hyperintense on T1w (a, g), hypointense on T2w (b, h) and show complete rim enhancement on T1w+Gd (c, i) images. The core of the lesion is hypointense on T1w (a, g), hyperintense on T2w (b, h) and may show restricted diffusion on DWI (d, j) and ADC maps (e, k). However, dynamic susceptibility contrast enhanced PWI does not show evidence of increased relative cerebral blood volume (rCBV) in the gadolinium-enhancing rim of the abscess (f) in comparison to the increased perfusion of the enhancing rim appreciable in the metastasis (white open arrow in l).
Magnetic resonance spectroscopy is helpful in the differential diagnosis of ring-enhancing lesions, especially between BAs and necrotic tumours (Figure 8). The normal spectrum of the brain tissue shows peaks corresponding to N-acetyl-aspartate and choline. Due to the lack of normal cell membranes and white matter in BAs, the main brain metabolites (N-acetyl aspartate, choline and creatine) are not seen, contrary to brain tumours, tumefactive demyelinating lesions, subacute infarct or vasculitis.
On the other hand, the central cavity of pyogenic BAs reveals peaks corresponding to lipids (0.8–1.2 ppm), lactate (1.3 ppm) and amino-acids (0.9 ppm).15 In particular, amino acids (valine, leucine and isoleucine) are typical of pyogenic abscesses but not always present. The presence of succinate and acetate peaks could suggest an anaerobic agent. Increases in lactate, acetate and succinate probably derive from the increased glycolysis and fermentation of the infecting micro-organisms. Amino acids (valine and leucine) are known to be the end products of proteolysis by enzymes released by neutrophils in pus. On the other hand, the presence of both lactate and lipid peaks is not specific of abscess. Indeed, they can also be observed in necrotic tumours.16
NUCLEAR MEDICINE IMAGING
The data show that 18 F-fluorodeoxyglucose positron emission tomography (18FDG-PET-CT) has limited specificity in distinguishing between neoplastic and non-neoplastic ring-enhancing intracerebral lesions (Figure 12) like pyogenic BAs, fungal abscesses, toxoplasmosis and tubercoloma.17 Indeed, it has a low specificity because the tracer is uptaken not only by inflamed tissues but also by malignant and healthy tissues that exhibit a high glucose metabolism.18,19
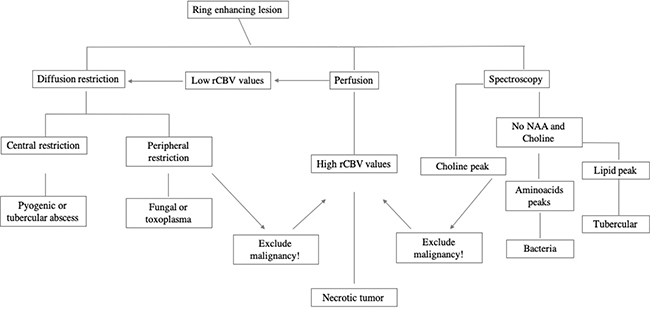
FIG 12. Flow-Chart for Differential Diagnosis between Brain Abscesses and Other Ring-Enhanced Lesions.
However, if signs and symptoms suggest an inflammatory pathology, there is an indication to perform a 18F-FDG-PET-CT with brain and total body acquisition according to the practice guidelines.20 Moreover, the 18F-FDG -PET-CT images, fused with conventional MRI sequences can be useful in assessing therapeutic responses to antibiotics treatment of BA and be helpful in optimising therapy.18
Finally, for the study of the CNS infections, data and European guidelines suggest performing the white blood cell (WBC) scintigraphy that shows high sensitivity and specificity. WBC scintigraphy is the most accurate nuclear medicine technique for CNS and head and neck infections. Whole-body, planar and SPECT/CT acquisitions can be mandatory especially in some low-grade infections.21
Differential Diagnosis
Overlap of MRI features between pyogenic BA and non-pyogenic abscesses (Mycobacterium tuberculosis, Toxoplasma, Aspergillus) and in some cases necrotic tumours can be present. Differential diagnosis with other lesions sometimes is very difficult by using conventional magnetic resonance imaging (cMRI) alone, and it can be improved by using advanced MRI techniques. A practical approach to the MRI differential diagnoses between pyogenic BAs and other brain lesions with a “ring-like” enhancement is presented in Figure 8.
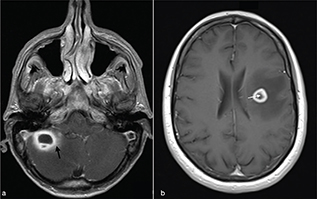
Necrotic brain tumours
These include high-grade gliomas (WHO grade IV) and metastases. They usually exhibit a T2w hypointense, irregular or incomplete, capsular rim.8 After injection of Gd, gliomas show non-homogeneous enhancement with some nodular areas (Figure 13). Metastases, on the other hand, can exhibit an enhancement pattern similar to pyogenic abscesses. However cystic neoplasms, often have a thicker medial margin if compared with pyogenic BA (Figure 6).9 Peripheral dark signals on SWI can be also found in glioblastomas and are related to the neoplastic intralesional neoangiogenesis and haemorrhage.8 As a rule, necrotic brain tumours have high ADC values. However low ADC values have been described in hyper-cellular tumour such as metastases from lung, breast, colorectal and testicular cancer (Figure 11).5 Moreover, necrotic tumours usually show an increase of neoangiogenesis with higher values of rCBV than abscesses in the periphery of the lesion.
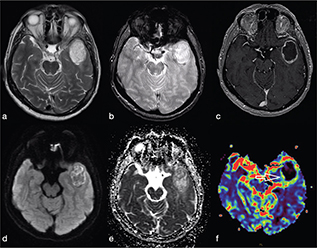
FIG 13. Necrotic Tumour in a 38-Year-Old Man: (a-c) a Left Temporal Lobe Cystic Mass is Shown. On T1w+Gd (c), the lesion shows irregular rim-enhancement. The central part of the lesion shows increased diffusivity (d, e) consistent with intratumoural necrotic degeneration. The rCBV map (f) showed increased perfusion within the enhancing rim of the lesion (open arrow). Final diagnosis was glioblastoma.
Tuberculoma and tuberculous abscesses
Tuberculous granuloma (tuberculoma) is the most common form of parenchymal CNS tuberculosis. As for pyogenic BA, the cMRI and DWI characteristics depend on the stage of infection: non-caseating, caseating with a solid centre or caseating with a liquid centre (see Table 2). Interestingly, caseating tuberculomas with a liquid centre have an elevated diffusion; indeed, any liquefaction of the central area of necrosis contains a clear fluid, as opposed to pus.7 SWI images may show a complete and regular hypointense peripheral ring.
TABLE 2. Conventional Magnetic Resonance Imaging and Diffusion-Weighted Imaging Characteristics of Tuberculous Granuloma (Tuberculoma) during the Different Stages of Infection
| Tuberculomas Stage |
T1-Weighted |
T2-Weighted |
Enhancement Pattern |
DWI |
| Noncaseating tuberculomas |
Hypointense |
Hyperintense |
Homogeneous and nodular |
No |
| Caseating tuberculomas with a solid centre |
Hypointense |
Hypointense |
Ring-like |
Restricted |
| Caseating tuberculomas with a liquid centre |
Hypointense |
Hyperintense |
Ring-like |
Elevated |
| DWI, diffusion-weighted imaging. |
Tuberculous BA are more similar to pyogenic BA compared to tuberculomas. They usually comprise a multiloculated cavity with central pus, with a thicker wall than a pyogenic BA. It must be distinguished from granuloma with central caseation and liquefaction mimicking pus (Figure 14). However, cMRI does not provide distinction between tubercular and pyogenic BA but lipid peaks without amino acids, on MR spectroscopy, are suggestive of mycobacteria.7
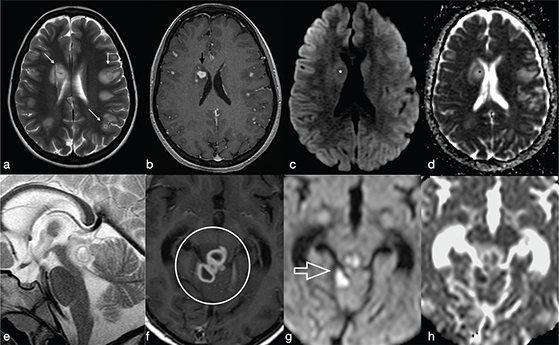
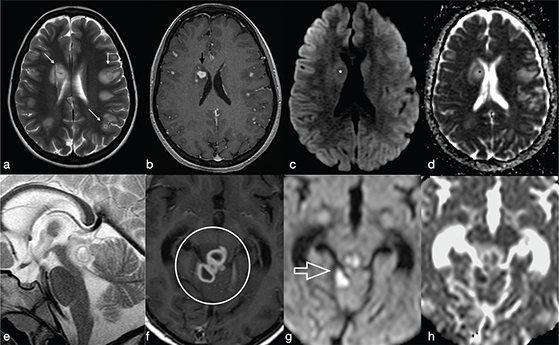
FIG 14. Tuberculoma (a–d) and Tubercular Abscess (e-h). Multiple tuberculomas in both cerebral hemispheres with an hypointense central dot (white arrows in a) within an hyperintense core on T2w are demonstrated. Nodular enhancement on T1+Gd is shown on smaller lesions while the larger one (black arrow in b) shows a thick ring delimitating a cystic core. On DWI and ADC map there is no restricted diffusion (asterisks in c-d). On the contrary, tubercular abscesses located in the quadrigeminal plate show a bright core on T2w, thick peripheral enhancement on T1+Gd (open circle in f) and restricted diffusion on DWI (g) and ADC maps (h).
Fungal abscesses
Fungal BA are rare and usually demonstrate low T2w signal in the centre and a ring-enhanced wall. Restricted diffusion may be seen in the capsule of the fungal abscess called “intracavitary projections.” Low ADC values are due to fungal organisms located at the periphery of the lesions and mucoid material.7 Opposite to pyogenic BA, fungal BA do not have the “dual rim” sign on SWI images but are characterised by a thick dark peripheral rim with multiple intralesional dark spots related to intralesional haemorrhage, typical in Aspergillus infection (Figure 15). Moreover, MRS may show lipid, lactate, amino acids and trehalose (3.6–8 ppm).15 In particular, trehalose has been observed in cryptococcosis.7
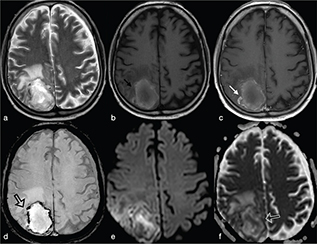
FIG 15. Fungal Brain Abscess (Aspergillus) in an Immunocompromised 44-Year-Old Man with Headache and Progressive Deterioration of Consciousness for 4 Days. A right parietal mass was observed in close proximity to the superior sagittal sinus with perifocal vasogenic oedema on T2w. (b, c) Spontaneous T1 shortening likely caused by xanthochromic fluid (extracellular methemoglobin) is present (b) with slight irregular enhancement after i.v. Gd administration (c). In fungal abscess, the rim of irregular hypointense signal on SWI, rather than haemoglobin breakdown products, may be consistent with the presence of elements with paramagnetic properties, such as iron or magnesium (d). DWI (e) and ADC maps (f) reveal heterogeneous signal with restricted diffusion in the lesional core and in the peripheral rim.
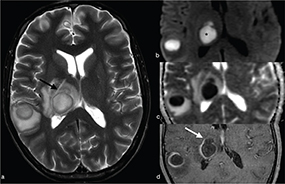
Cerebral toxoplasmosis
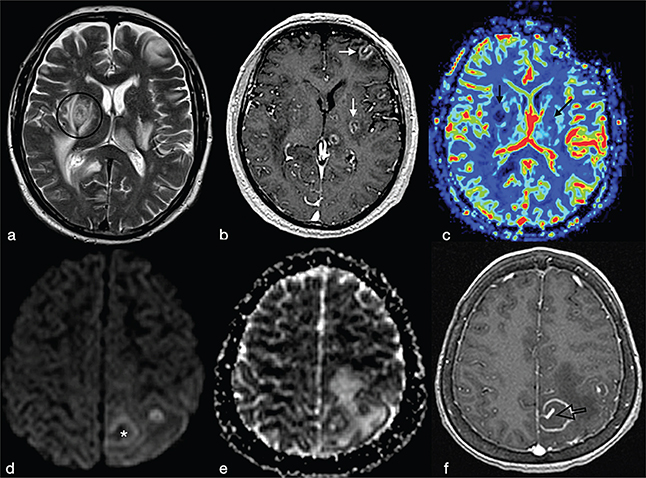
Cerebral toxoplasmosis is typical of immunocompromised patients. MRI shows multiple lesions in different stages of evolution typically located in the subcortical and periventricular white matter, in the basal ganglia and thalami. In particular, two signs are recognised as typical of toxoplasmosis: the “concentric” target sign (concentric alternating hypointense and hyperintense rims in T2w images), and the “eccentric” target sign (peripheral rim of enhancement and focal lateral eccentric enhancing nodule on T1w post-contrast) (Figure 16). On DWI, the centre of the toxoplasma abscess is seen to have ADC values higher than in pyogenic abscesses.22
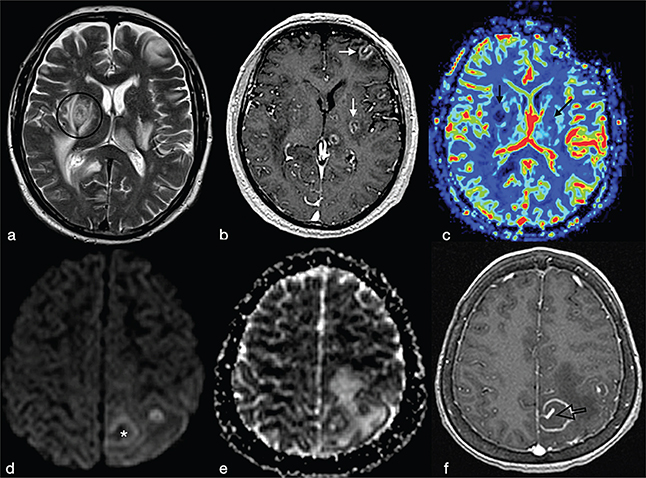
FIG 16. Multiple Toxoplasma gondii Abscesses in a 45-Year-Old Immunocompromised Woman. T2w (a), T1+Gd (b, f), rCBV map (c), DWI (d) and ADC map (e). Multiple supratentorial brain abscesses in various stages of development with enhancing asymmetric nodules after Gd-injection (“eccentric target sign”) (arrows) can be observed (b, f). Note also the concentric alternating zones of hypo- and hyperintensities on T2w: “concentric target sign” (circle in a). Toxoplasma gondii abscesses typically do not show a core of restricted diffusion on DWI (asterisk in d) while low ADC values may be seen in the capsule (e).
CONCLUSIONS
BA are common manifestations of CNS infections. Conventional magnetic resonance imaging together with advanced sequences can suggest the diagnosis and management of BAs. Adding more advanced sequences such as DWI, PWI and MR spectroscopy to the cMRI protocol will increase the diagnostic confidence. However, in daily practice it may sometimes be difficult to perform all the advanced MRI techniques in each patient. Of note, DWI is routinely performed in every MRI protocol in the diagnosis of brain focal lesions and helps in the differential diagnosis. On the other hand, MRS and PWI should be used in selected cases when there is doubt about the diagnosis.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
FUNDING
The authors received no funding.
DATA AVAILABILITY STATEMENT
No datasets were generated for this review.
COMPLIANCE WITH ETHICAL STANDARDS
No ethics approval needed for this review.
REFERENCES
- Osenbach RK, Loftus CM. Diagnosis and management of brain abscess. Neurosurg Clin North Am. 1992;3:403–420. https://doi.org/10.1016/S1042-3680(18)30671-5
- Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess: Systematic review and meta-analysis. Neurology. 2014;82:806–13; https://doi.org/10.1212/WNL.0000000000000172
- Osborn AG, Hedlund GL. Congenital, acquired pyogenic, and acquired viral infections. In Osborn’s brain, imaging, pathology, and anatomy, 2nd ed. Salt Lake City, UT: Elsevier, Inc.; 2017. p. 353–8.
- Brouwer MC, Tunkel AR, McKhann GM 2nd, van de Beek D. Brain abscess. N Engl J Med. 2014 Jul 31;371:447–56. https://doi.org/10.1056/NEJMra1301635
- Muccio CF, Caranci F, D’arco F, et al. Magnetic resonance features of pyogenic brain abscesses and differential diagnosis using morphological and functional imaging studies: A pictorial essay. J Neuroradiol. 2014 Jul;41(3):153–67. https://doi.org/10.1016/j.neurad.2014.05.004.
- Haimes AB, Zimmerman RD, Morgello S, et al. MR imaging of brain abscesses. Am J Roentgenol. 1989;152:1073–85. https://doi.org/10.2214/ajr.152.5.1073
- Luthra G, Parihar A, Nath K, et al. Comparative evaluation of fungal, tubercular, and pyogenic brain abscesses with conventional and diffusion MR imaging and proton MR spectroscopy. Am J Neuroradiol. 2007;28:1332–8. https://doi.org/10.3174/ajnr.A0548.
- Toh CH, Wei KC, Chang CN et al. Differentiation of pyogenic brain abscesses from necrotic glioblastomas with use of susceptibility-weighted imaging. Am J Neuroradiol. 2012;33:1534–8. https://doi.org/10.3174/ajnr.A2986
- Karampekios S, Hesselink J. Cerebral infections. Eur Radiol. 2005;15:485–93; https://doi.org/10.1007/s00330-004-2556-1
- Antulov R, Dolic K, Fruehwald-Pallamar J, et al. Differentiation of pyogenic and fungal brain abscesses with susceptibility-weighted MR sequences. Neuroradiology. 2014;56:937–45. https://doi.org/10.1007/s00234-014-1411-6.
- Muccio CF, Esposito G, Bartolini A, et al. Cerebral abscess and necrotic cerebral tumours: Differential diagnosis by perfusion-weighted magnetic resonance imaging. Radiol Med. 2008;113:747–57. https://doi.org/10.1007/s11547-008-0254-9.
- Cartes-Zulmelzu FW, Stavrou Ioannis, Castillo M, et al. Diffusion-weighted imaging in the assessment of brain abscesses therapy. Am J Neuroradiol. 2004;25:1310–17.
- Finelli PF, Foxman EB. The etiology of ring lesions on diffusion-weighted imaging. Neuroradiol J. 2014 Jun;27(3):280–7. https://doi.org/10.15274/NRJ-2014-10036.
- Hartmann M, Jansen O, Heiland S, et al. Restricted diffusion within ring enhancement is not pathognomonic for brain abscess. Am J Neuroradiol. 2001;22:1738–42.
- Gupta RK, Jobanputra KJ, Yadav A. MR spectroscopy in brain infections. Neuroimag Clin N Am. 2013;23:475–98. https://doi.org/10.1016/j.nic.2013.03.004.
- Chiang IC, Hsieh TJ, Chiu ML, et al. Distinction between pyogenic brain abscess and necrotic brain tumour using 3-tesla MR spectroscopy, diffusion and perfusion imaging. Br J Radiol. 2009 Oct;82:813–20. https://doi.org/10.1259/bjr/90100265.
- Rahmana TW, Walea DJ, Vigliantia BL, et al. The impact of infection and inflammation in oncologic 18F-FDG PET/CT imaging. Biomed Pharmacother. 2019;117:109168. https://doi.org/10.1016/j.biopha.2019.109168
- Dethy S, Manto M, Kentos A, et al. PET findings in a brain abscess associated with a silent atrial septal defect. Clin Neurol Neurosurg. 1995;97:349–53. https://doi.org/10.1016/0303-8467(95)00067-T
- Tsuyuguchi N, Sunada I, Ohata K, et al. Evaluation of treatment effects in brain abscess with positron emission tomography: Comparison of fluorine-18-fluorodeoxyglucose and carbon-11-methionine. Ann Nucl Med. 2003;17:47–51. https://doi.org/10.1007/BF02988258
- Jamar F, Buscombe J, Chiti A, et al. EANM/SNMMI guideline for 18F-FDG use in inflammation and infection. J Nucl Med. 2013;54:647–58. https://doi.org/10.2967/jnumed.112.112524
- Signore A, Jamar F, Israel O, et al. Clinical indications, image acquisition and data interpretation for white blood cells and anti-granulocyte monoclonal antibody scintigraphy: An EANM procedural guideline. Eur J Nucl Med Mol Imag. 2018;45:1816–31. https://doi.org/10.1007/s00259-018-4052-x
- Roche AD, Rowley D, Brett FM, et al. Concentric and eccentric target MRI signs in a case of HIV-associated cerebral toxoplasmosis. Case Rep Neurol Med. 2018:9876514:3. https://doi.org/10.1155/2018/9876514