Original Article
Iffat Jahan1, Momtaz Begum2, Shahin Akhter2, Zakirul Islam3, Mainul Haque4, and Nusrat Jahan5
1Department of Physiology, Eastern Medical College, Cumilla, Bangladesh
2Department of Physiology, Chittagong Medical College, Chattogram, Bangladesh
3Department of Pharmacology, Eastern Medical College, Cumilla, Bangladesh
4Universiti Pertahanan Nasional Malaysia (National Defence University of Malaysia), Kuala Lumpur, Malaysia
5Department of Internal Medicine, United Hospital, Dhaka, Bangladesh
Alternate nostril breathing (ANB) is one of the best and easiest breathing exercises. ANB exercise has beneficial effects on cardiac function in healthy and diseased people. The objectives of this study were to assess the effects of ANB exercise on cardiac physiology among healthy medical students. This was a prospective interventional study that was conducted in the Department of Physiology, Chittagong Medical College (CMC), Chattogram, Bangladesh, from July 2017 to June 2018. A total of 100 research participants (RPs) aged 18–20 years, Year-I medical students of CMC, were selected. A simple random sampling method was adopted. The selection was done after the inclusion and exclusion criteria were applied. The age and body mass index (BMI) of the RPs were analogous in both the control and experimental groups. Cardiac parameters, like pulse and blood pressure (BP), were measured. The initial baseline data were recorded for both groups and after 4 weeks. The research respondents of the experimental group performed ANB exercise for 4 weeks. The mean value pulse and BP were significantly (p < 0.001) changed after breathing exercise, compared to the values before the breathing exercise. The results of this study suggest that cardiac function significantly improves after the breathing exercise. Therefore, ANB can be recommended for increasing cardiac efficiency.
Keywords: alternate nostril, nose, breathing exercise, ANB, cardiac function, healthy young adults, Chattogram Medical College, CMC
Global health-related issues have been significantly changed in the last 100 years because of changes in lifestyles to cope with the new social order. Then, stress became a major cause of multiple noncommunicable diseases around the world that increases both morbidity and mortality by minimizing the quality of life.1–4 In Bangladesh, around 20% of the adult population are suffering from cardiac disorders, especially hypertension.5 Good health status, both physiological and psychological, is dependent, to a great extent, on good cardiac performance. In addition, good lifestyle habits, especially regular yoga practice, maintain a high quality of health.2,6 Preventive, curative, and promotive health practices have been much advocated to achieve optimum health status.7 The breathing function is one that is possible to consciously control among all the autonomic functions and is widely accepted as a promising method to ensure health and fitness.8,9 It provides more oxygen, and emits out carbon-di-oxide and other toxic gaseous substances.9 Controlled breathing channels the sympathetic and parasympathetic physiologic functions toward a harmonic state.8 Multiple earlier studies reported that alternate nostril breathing (ANB) modulated the sympathovagal balance to augment better-quality cardiac function.4,8–10 ANB also relieved stress,11–13 refined metabolism,14–20 improved cognitive function,11,21–23 and delayed the normal aging process.24,25 Breathing exercises are often called pranayama in Indian yoga-related manuscripts.10 Yoga is a psycho-somatic spiritual performance that frequently achieves, merges, and harmonizes between the mind, body, and soul2 and has been widely practiced in the Indian subcontinent for over thousands of years.10 Yoga gained importance and became increasingly accepted as an overall health improvement tool in the Western society.26,27 Thereafter, the United Nations General Assembly in 2015 declared June 21 as the “International Yoga Day”.28 Different types of breathing exercises that include deep breathing, inhalation–retention–exhalation at fixed intervals, abdominal/diaphragmatic breathing, and ANB/Anuloma Viloma were practiced in different disciplines.7 ANB is one of the easiest and the best breathing exercises.9 In addition, it is cost-effective, as it does not require any special equipment or definitive time.9 ANB completely rejuvenates and energies the physiological process that includes both the physical and the psychological domains.2,9 In ANB exercise, slow inhalation followed by slow exhalation of air through one nostril is practiced keeping the alternate nostril closed with a short interval of breath-holding in between inhalation and exhalation.29 The burden of the medical curriculum frequently imposes extreme study-related stress on the medical student.4,30 Subsequently, continuous stress recurrently leads to irritability, insomnia, anxiety, and depression.4 Stress even changes the set point of the hypothalamic–pituitary axis, leading to sympathovagal imbalance.8 Stress has immediate harmful effects on the cardiovascular system. Hence, cardiovascular disease is often prevalent among these individuals.8 Multiple studies revealed that deep breathing exercise significantly decreased salivary cortisol concentration, and thereby blood pressure (BP); had a neuroprotective effect; increased skill, memory with decreased anxiety; improved cognitive functions and the lipid profile among high-risk patients of dyslipidemia.11,12,18–20,21–23 In previous studies, breathing exercise revealed that it improved significantly both heart rate (HR) and BP among healthy and poor cardiovascular performers by minimizing stress.4, 8,30–33 Breathing exercise resets the autonomic nervous system with decreased adrenalin-mediated sympathetic activity and thereby peripheral resistance, HR, and BP.8,31–34 ANB was used effectively for preventive and therapeutic purposes, either alone or in combination with pharmacological interventions.2 Regular practicing of ANB has been reported to produce positive cardiovascular system impact by preventing the onset of multiple cardiovascular disease and progression.2 This study was conducted to assess the physiological effects of short-term ANB exercise on cardiac function among healthy medical students.
This research work was an experimental study. It was conducted in the Department of Physiology, CMC, Chattogram, Bangladesh, from July 2017 to June 2018. A total of 100 research participants (RPs) were recruited for this study, with 50 members each in the control and experimental groups, respectively. RPs were Year-I medical students of CMC, aged 18–20 years, with a BMI of 18.5–22.9 kg/m2, enrolled in the study with informed consent. Simple random sampling by lottery method was adopted to select all the RPs.
To determine the sample size for this study, the following formula was used:35,36
n = the desired sample
Zα= Z value of the standard normal deviate set at 1.96 that corresponds to the 95% confidence interval
Zβ= Z value of standard normal deviate at 80% power
σ = The standard deviation of the population (from the previous study) 37
μ1 = Expected control group mean (from the previous study) (37)
μ2 = Expected experimental group mean (from the previous study) (37)
Here,
Zα = 1.96, Zβ =0.84, σ = 8.46, μ1 = 85.70, μ2= 90.43
Thereby, 50 students in the control and experimental groups were selected as study subjects. Ten students dropped out during the study. Ten percent of extra students (total 110) were taken to mitigate the dropping out of the subjects.
The Year-I medical students of CMC, Chattogram, aged between 18 and 20 years, having a BMI of 18.5–22.9 kg/m2, and fulfilling the inclusion and exclusion criteria, were enrolled in the study with informed consent. Detailed personal information, medical and family history, and the history of physical activity status were recorded in a pre-determined questionnaire from all the RPs who participated voluntarily. The RPs, who previously did not perform breathing exercises, were randomly selected.
RPs with a previous history of cardiovascular disease, respiratory illness, any nasal pathology, and smoking, and those receiving respiratory depressant drugs, and those with vertebral deformities were excluded from the study.
Age, height, body weight, and the BMI of the RPs were recorded in a predesigned case record form. BMI was calculated by the formula, BMI = Weight in Kg/height in m2. Cardiac parameters (pulse and BP) of students were recorded in an upright sitting posture before commencing breathing exercises to see the baseline parameters in both the control and experimental groups. The control group RPs were neither trained nor allowed to practice ANB, and the experimental group RPs were taught detailed steps of ANB with audiovisual demonstration, and they practiced ANB daily 10 min during the college period for 4 weeks. Radial pulse was counted for a minute keeping the subject’s forearm slightly pronated. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured in the sitting position in the left arm of each subject by a palpatory and auscultatory method with the help of a stethoscope and aneroid sphygmomanometer after proper exposure (ALPK2, Japan). RPs were asked to remain in the sitting posture for 15 min to become mentally and physically relaxed and free from excitation and anticipation. Three consecutive readings from pulse and BP measurement procedures were taken, and the best value was recorded. Then, the experimental group practiced ANB exercise daily for 10 min for 4 weeks. After 4 weeks, cardiac parameters were again measured in both the control and experimental groups.38
Detailed personal information, medical and family history, and the history of physical activity status were recorded in a pre-determined questionnaire from all the RPs who participated voluntarily.
All the data were compiled and processed after collection. Results were expressed as mean ± SD (standard deviation) and range. Pulse and BP records were analyzed by the independent t-test in SPSS-23 (IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.). A paired-sample t-test compared between pre- and post-intervention data and unpaired t-test compared between the groups for statistical analysis. 95% confidence limit was taken as a minimum level of significance. In the interpretation of results, p < 0.05 was accepted as the level of significance.
The protocol of this study was approved by the members of the Ethical Review Board (ERB) of CMC, Chattogram, and received a certificate of ethical clearance of ERB [Reference No.: CMC/PG/2018/403; dated 10/5/2018].
In this study, all experimental RPs were like healthy control by age, height, weight, and BMI. In this study, at baseline, pulse, SBP, and DBP between the control and experimental groups at the beginning of the study showed no significant difference (Table 1). Again, significant decrement (p < 0.001) was observed in all these cardiac parameters between the control and experimental groups at the end of the study (Table 2).
| Cardiac attributes | Pulse (beats/min)Mean ± SD(range) | SBP (mm of Hg)Mean ± SD(range) | DBP (mm of Hg)Mean ± SD(range) | |
|---|---|---|---|---|
| At the beginning of study | Control group (n = 50) | 78.76 ± 1.890 (74–86) |
116.00 ± 4.949 (110–120) |
75.40 ± 5.425 (60–80) |
| Experimental group (n = 50) | 78.92 ± 1.904 (72–84) |
115.80 ± 4.986 (110–120) |
74.20 ± 6.091 (60–80) |
|
| p-value (t-value) | 0.667 ns (0.433) |
0.844 ns (0.198) |
0.278ns (1.098) |
|
| At the end of study | Control group (n = 50) | 79.32 ± 2.478 (68–82) |
117.40 ± 4.431 (110–120) |
76.30 ± 5.230 (60–80) |
| Experimental group (n = 50) | 72.72 ± 4.329 (62–80) |
103.40 ± 6.884 (90–110) |
68.36 ± 6.574 (60–80) |
|
| p-value (t-value) | <0.001** (9.423) |
<0.001** (12.537) |
<0.001** (7.394) |
|
| Data expressed as mean ± SD, ANB = alternate nostril breathing, SBP = systolic blood pressure, DBP = diastolic blood pressure, SD = standard deviation; Figures in parenthesis indicate range, statistical analysis done by Student’s unpaired t-test, ns = not significant, ** = statistically significant test (p < 0.001). | ||||
| Cardiac attributes | Pulse (beats/min) Mean ± SD (range) |
SBP (mm of Hg) Mean ± SD (range) |
DBP (mm of Hg) Mean ± SD (range) |
|
|---|---|---|---|---|
| Control group (n = 50) |
At the beginning of study | 78.76 ± 1.890 (74–86) |
116.00 ± 4.949 (110–120) |
75.40 ± 5.425 (60–80) |
| At the end of study | 79.32 ± 2.478 (68–82) |
117.40 ± 4.431 (110–120) |
76.30 ± 5.230 (60–80) |
|
| p-value (t-value) |
0.159 ns (1.429) |
0.181 ns (1.358) |
0.441 ns (0.777) |
|
| Experimental group (n = 50) |
At the beginning of study | 78.92 ± 1.904 (72–84) |
115.80 ±4.986 (110–120) |
74.20 ± 6.091 (60–80) |
| At the end of study | 72.72 ± 4.329 (62–80) |
103.40 ± 6.884 (90–110) |
68.36 ± 6.574 (60–80) |
|
| p-value (t-value) |
<0.001** (11.616) |
<0.001** (12.246) |
<0.001** (5.496) |
|
| Data expressed as Mean ± SD, ANB = alternate nostril breathing, SBP = systolic blood pressure, DBP = diastolic blood pressure, SD = standard deviation; Numbers in parenthesis indicate range, statistical analysis done by Student’s paired t-test, ns = not significant (p > 0.05), ** = statistically significant test (p < 0.001). | ||||
After 4 weeks’ follow-up, the experimental group with ANB exercise experienced a significant decrease in their pulse, SBP, and DBP (p < 0.001) when compared to their baseline values, whereas after 4 weeks the control group, which had no exposure to ANB, did not experience any significant changes in the above-mentioned parameters (Table 2 and Figures 2, 3).
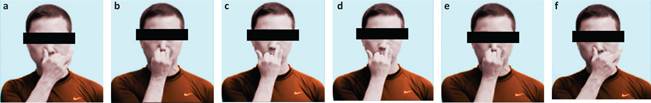
FIG 1. Steps of ANB. (a) The RPs were asked to close the left nostril with the thumb of the left hand and inhale through the right nostril for 6 sec. (b) Then, they closed the right nostril by the index finger and held the breath for 6 sec. (c) Then, they exhaled through the left nostril slowly for 6 sec. (d) Then, they inhaled through the left nostril, keeping the right nostril closed for 6 sec. (e) Then, the RPs hold the breath, closing both nostrils for 6 sec. (f) Then, they exhaled through the right nostril, keeping the left closed for 6 sec.38

FIG 2. Cardiac Parameters in the Control Group (without ANB Exercise) at the Beginning and End of the Study.
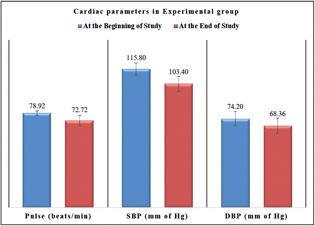
FIG 3. Cardiac Parameters in the Experimental Group (with ANB exercise) at the Beginning and End of the study.
This study assessed cardiac functions in the experimental group before and after ANB exercise for 4 weeks by analysis of pulse, SBP, and DBP, and compared these results with the control group. In this study, in the control group, the pulse rate, SBP, and DBP were observed. The mean pulse rate, SBP, DBP in the control group before and after 1 month without practicing ANB did not show any change. Although these parameters were a bit higher than the previous values, they were insignificant. In the experimental group, cardiac parameters (pulse rate, SBP, and DBP) before and after ANB for 1 month were significantly decreased. Previous investigators also reported similar findings.2,4,8,29–31,39–43 The results of this study were identical with the conclusions from Biswas et al.2 Pal et al.4 and other investigators. They supposed that breathing exercises might increase parasympathetic activity and decrease sympathetic activity. This might cause a decrease in pulse rate and BP.2,44
During breathing exercise, attention on the act of breathing removes focus from worldly worries and de-stresses a person.38,41,45 This may decrease the release of adrenaline and reduce BP, which was explained by Gupta et al.45 and Dhungel et al.39 Breathing exercise alters the hypothalamic discharge, leading to a decrease in sympathetic tone and peripheral resistance. Hence, the DBP was decreased. Increase in vagal tone reduces the workload on the heart and thus decreases CO and thereby SBP.41 Regular practice of rhythmic slow breathing has been shown to increase baroreflex sensitivity activation and thus reduce SBP and DBP in hypertensive patients.46 Possibly, the above mechanisms were also responsible for the reduction in the cardiac parameters in this study. Some investigators found no significant changes in SBP and DBP after breathing exercise practice, which is dissimilar with the current research.47 It was explained in earlier researches that RPs were normotensive due to the short period of study.47 ANB exercise brought about a significant decrement in cardiac parameters (pulse, BP) in the experimental group of medical students. Therefore, ANB is very much helpful for the improvement of cardiac function as well as the prevention of different complications of cardiac problems.
This study was conducted for both academic and clinical purposes in a short period of time. Although optimal care was taken by the researcher in every step of the study, there were some limitations: (1) short period of study, (2) small sample size that might not represent the whole community, (3) study conducted with a limited age group, (4) study conducted only on Year-I medical students, (5) a socio-demographic study not conducted, (6) proper sitting posture in the floor on the mat was not maintained and (7) catecholamine level in the blood and urinary excretion were not measured to observe the stress pattern.
In the present study, yoga-based ANB exercise for 1 month brought about significant improvement in the cardiac parameters (pulse and BP) in the RPs. Although, it was difficult to comment on the exact mechanism involved here, probably it was due to the shifting of the sympathovagal balance toward parasympathetic predominance. Therefore, this study concludes that the regular performance of ANB can be a useful measure for the improvement of cardiac endurance and functions. This may help in preventing different complications of cardiac problems in the future. As this procedure requires no instrument, is a straightforward technique to adopt, and a cost-effective phenomenon, popularization of this activity will ultimately be helpful in increasing the longevity of human beings.
The authors report no conflict of interest.
This study had no financial support.
The authors acknowledge the Department of Physiology, CMC, Chattogram, for the kind cooperation during sample collection and allowing them to use laboratory instruments. The authors are also thankful to the RPs for their active, sincere, and voluntary participation. In addition, the authors are grateful to Professor (Dr.) M. S. Razzaque of Lake Erie College of Osteopathic Medicine, Pennsylvania, USA, for his helpful suggestions.
The data will be available only for research purpose.
This study was approved by the Chittagong Medical College, Institutional Review Board, Chattogram, Bandladesh.