Original Research
Effects of alternate nostril breathing exercise on respiratory functions in healthy young adults leading stressful lifestyle
Iffat Jahan1, Momtaz Begum2, Shahin Akhter2, Md. Zakirul Islam3, Nusrat Jahan4 and Mainul Haque5
1Department of Physiology, Southern Medical College, Chattogram, Bangladesh
2Department of Physiology, Chittagong Medical College, Chattogram, Bangladesh
3Department of Pharmacology, Eastern Medical College, Cumilla, Bangladesh
4Department of Internal Medicine, United Hospital, Dhaka, Bangladesh
5Unit of Pharmacology, Faculty of Medicine and Defence Health, Universiti Pertahanan Nasional Malaysia (National Defence University of Malaysia), Kuala Lumpur, Malaysia
Corresponding author: runurono@gmail.comSubmitted: 21 January 2020. Accepted: 27 February 2020. Published: 19 March 2020.DOI: 10.15586/jptcp.v27i1.668
ABSTRACT
Alternate nostril breathing (ANB) is one of the best and easiest breathing exercises (pranayama) of yoga that are good for health and physical fitness. ANB exercise has beneficial and therapeutic effects on respiratory function in both normal as well as diseased humans. This study was conducted with the objective of assessing the physiological effects of short-term ANB exercise on respiratory function in healthy adult individuals leading a stressful life. This prospective interventional study was conducted in the Department of Physiology, Chittagong Medical College (CMC), Chattogram, Bangladesh from July 2017 to June 2018. A total of 100 participants aged 18–20 years, studying in the first year in CMC, were included by using a simple random sampling method. Among them, 50 participants were enrolled in the experimental group. Age- and BMI-matched 50 participants constituted the control group. Height, weight were measured, and BMI was calculated. The participants of the experimental group performed ANB exercise over 4 weeks for 10 min/day. The control participants were neither trained nor allowed to practice nostril breathing during the whole study period. Respiratory parameters like forced vital capacity (FVC), forced expiratory volume in 1st second (FEV1), and peak expiratory flow rate (PEFR) were measured by using a digital spirometer (Chest graph HI-101, Japan). Readings were taken in a healthy upright sitting posture in the control and experimental group initially and after 4 weeks. Student’s t-test was conducted by using SPSS for windows version-23. The mean value of FVC, FEV1, PEFR were significantly (P < 0.001) changed after the ANB exercise when compared to the values before breathing exercise. The results of this study suggest that respiratory function is significantly improved after the ANB exercise. Therefore, ANB can be recommended for increasing respiratory efficiency.
Keywords: alternate nostril, nose, breathing exercise, yoga, pranayama, respiratory function, healthy young adults
INTRODUCTION
Good health is the greatest asset of human life.1 Proper diet, adequate exercise, and a stress-free life are essential to maintain good health.1 Rapid industrialization, environmental pollution, overcrowding, and sedentary lifestyles are responsible for the deterioration of the health of a person.2 WHO predicts that physical or mental stress will become the second leading cause of disability and cardio-respiratory disease morbidity by the year 2020.3 Atmospheric pollution is responsible for various types of respiratory diseases.1 Dust allergy, common cold with cough, chronic obstructive pulmonary disease (COPD), bronchial asthma, status asthmaticus are common diseases nowadays especially in city areas.1 In Bangladesh, approximately 11.4% of COPD is prevalent in the urban population comprising people aged over 35 years and 6.8% of this population suffers from bronchial asthma in coastal region.4,5 Physical health, mental health, and fitness depend mainly on respiratory endurance.6 Some specific techniques are required to improve our physical and mental abilities in everyday life.2 Preventive, curative, and promotive health in medical science is quite useful to achieve optimum physical and psychological fitness.7 Among all the autonomic functions of our body, the breathing function can be consciously controlled.8 Consciously controlled breathing or pranayama is widely admired as a promising technique.9 It enhances the mental and physical power of the human body.9 It also provides oxygen and expires out carbon-di-oxide and other unwanted toxic gaseous substances from the body.9 Controlled breathing can help to bring the sympathetic and parasympathetic functions into a harmonic state.8 Breathing exercises (Pranayama) like alternate nostril breathing (ANB) are gaining importance and becoming increasingly accepted in Western society.10,11 In previous studies, it was found that ANB modulated sympathovagal balance with improved respiratory function.8,9,12,13 It also relieved stress 14–16 and refined metabolism.17–23 It also increased cognitive function 14,24–26 and attenuation of healthy aging.27,28 Among different types of breathing exercises (pranayama), ANB is one of the best and easiest breathing exercises.9 It is cost-effective and does not require any special equipment or time investment.9 It completely purifies the body as well as mind.2,9 It also promotes health and fitness.2,9 ANB produces consistent positive physiological changes and has a sound scientific basis for its beneficial outcomes in the human body.6 While doing the ANB exercise, slow inhalation followed by slow exhalation of air through one nostril is practiced keeping the alternate nose closed with a short interval of breath-holding in between breathing and exhalation.29 Different studies observed beneficial effects of breathing exercise on diseased as well as normal healthy subjects.7,18,30–35 In a study, an 18% improvement of O2 consumption was observed after 1 month of doing the ANB exercise.17 Significantly increased VO2 max (maximal oxygen uptake) and basal metabolic rate were noted after completion of the deep breathing exercise in healthy participants and medical students.6,18 Medical students lead a stressful study life as stated in different studies.12,35 The burden of the medical curriculum imposes extreme study stress on the medical student.12,35 Continuous mental-pressure can lead to irritability, insomnia, anxiety, and depression.12 Mental stress can change the set point of the hypothalamic–pituitary axis leading to sympathovagal imbalance.8 It may cause immediate harmful effects on the respiratory rate, and thus, respiratory diseases may set in.8 Respiratory muscles undergo work hypertrophy with maximum functioning during breathing exercises like ANB.7,36 A significant improvement was noted for forced vital capacity (FVC), forced expiratory volume in 1st sec (FEV1), maximum expiratory pressure (MEP), maximum inspiratory pressure (MIP), peak expiratory flow rate (PEFR), expiratory reserve volume (ERV) among healthy young subjects and also on healthy medical students.7,13,31,34 The increase in MEP and MIP in the yoga group indicates that yoga improves the strength of both expiratory and inspiratory muscles.33 This study was conducted with the aim to assess the physiological effects of short-term ANB exercise on respiratory function in healthy adult individuals under stressful conditions.
MATERIALS AND METHODS
Study Design
This research was an experimental study that was conducted in the Department of Physiology, CMC, Chattogram, Bangladesh, under continuous supervision and monitoring during the period from July 2017 to June 2018.
Study Sample
A total of 100 participants were recruited in this study, 50 in each of the control and experimental group.
Sampling Method
Simple random sampling by lottery method was adopted as the method to select all the subjects.
Study Period
The study was conducted over a period from July 2017 to June 2018.
Study Area
Department of Physiology, CMC, Chattogram, Bangladesh.
Inclusion Criteria
The first-year students aged between 18 and 20 years having BMI 18.5–22.9 kg/m2 and studying in CMC, Chattogram, fulfilling the inclusion and exclusion criteria were enrolled in the study with informed consent. Detailed personal information, medical and family history, and the history of physical activity status was recorded in a pre-fixed questionnaire given to all the participants who participated voluntarily. Participants who previously did not perform breathing exercises were randomly selected.
Exclusion Criteria
Students with previous history of cardiovascular, respiratory illness, having any nasal pathology, smokers, participants receiving respiratory depressant drugs, and vertebral deformities are excluded from the study.
Experimental Details
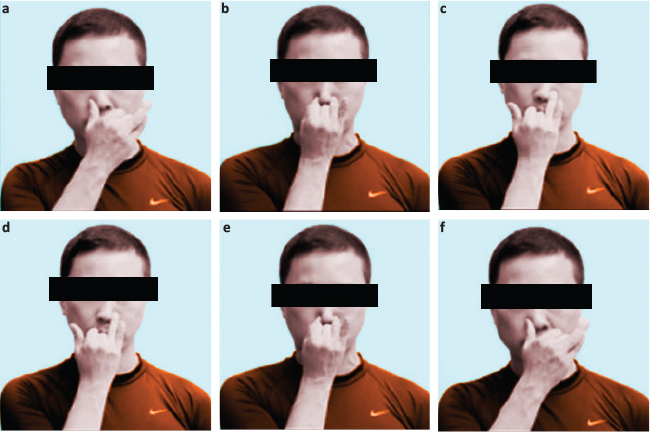
Age, height, body weight, and BMI of the participants were recorded in a predesigned case record form. Respiratory parameters (FVC, FEV1, and PEFR) of students were registered in upright sitting posture before commencing breathing exercises to see the baseline parameters in the both control and experimental groups by using a digital spirometer (Chest graph, HI-101, Japan). The readings of measured predicted, and percentage of predicted values of FVC, FEV1, and PEFR were noted from the spirometer monitor. Three consecutive readings were taken, and the best value was noted on tracing paper. Control group participants were neither trained nor allowed to practice in ANB exercises and experimental group participants were taught the detailed steps of ANB with audio-visual demonstration and they practiced ANB daily for 10 min during the college period for 4 weeks (Figure 1).
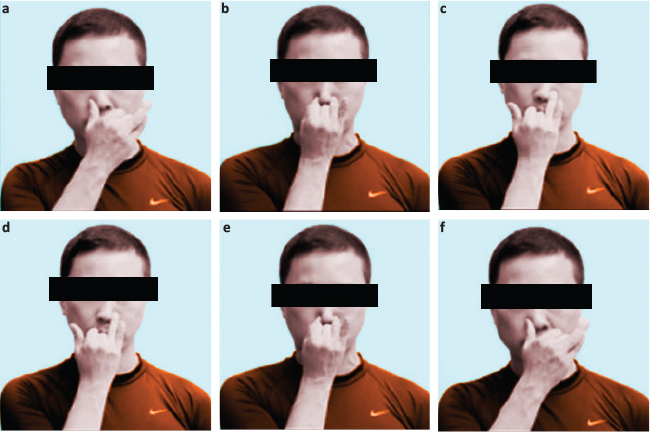
FIG 1. Steps of Alternate Nostril Breathing Exercise (ANB) (a) The subjects were asked to close the left nostril with the thumb of the left hand and inhale through the right nostril for 6 sec. (b) Then they closed the right nostril by using the index finger and held their breath for 6 sec. (c) After that they exhaled through the left nostril slowly for 6 sec. (d) Then they inhaled through the left nostril, keeping the right nostril closed for 6 sec. (e) Then the Subjects hold their breath, closing both nostrils for 6 sec. (f) Then they exhaled through the right nostril, keeping the left closed for 6 sec.37
After 4 weeks, respiratory parameters were again measured for both the control and experimental group.
Data Collection Details
Detailed personal information, medical and family history, and the history of physical activity status were recorded in a pre-fixed questionnaire given to all the participants who participated voluntarily.
Statistical Analysis
All the data were compiled and processed after collection. Results were expressed as mean ± SD (standard deviation) and range. FVC, FEV1 and PEFR data were analyzed by Student’s t-test using SPSS-23. For statistical analysis, a paired-sample t-test was used to compare respiratory parameters at the beginning and the end of the study in control (without ANB exercise) and experimental groups (with ANB exercise) and unpaired t-test was used to compare between control (without ANB exercise) and experimental groups (with ANB exercise) at the beginning and the end of the study. Ninety-five percent confidence limit was taken as a minimum level of significance. In the interpretation of results, P < 0.05 was accepted as the level of significance.
Ethical Approval
The protocol of this study was approved by the members of the Ethical Review Board of CMC, Chattogram, Bangladesh, and received a certificate of ethical clearance of ERB [Reference No.: CMC/PG/2018/403. Dated 10/5/2018].
RESULTS
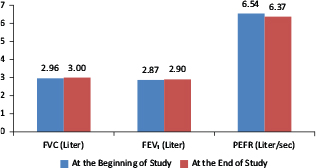
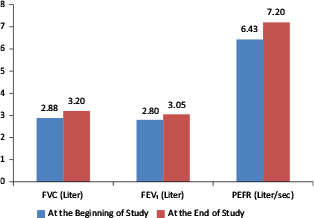
In this study, all experimental participants were healthy controls based on age, height, weight, and BMI. In this study, at baseline, FVC, FEV1, and PEFR values the between control and experimental group at the beginning of the study showed no significant difference (Table 1). Again, the significant increment was observed in all these parameters between the control and experimental group at the end of the study (Table 1). After 4 weeks of follow-up, an experimental group with ANB exercise had significantly increased FVC, FEV1, and PEFR values (P < 0.001) when compared to their baseline values, whereas after 4 weeks without ANB in the control group all these parameters showed no significant changes (Table 2; Figures 2 and 3).
TABLE 1 Comparison of Respiratory Parameters between Control (without ANB Exercise) and Experimental Group (with ANB Exercise) at the Beginning and at the End of the Study (n = 100)
| Respiratory Attributes |
|
FVC (Liter) Mean ± SD (Range) |
FEV1 (Liter) Mean ± SD (Range) |
PEFR (Liter/sec) Mean ± SD (Range) |
| At the beginning of study |
Control group (n = 50) |
2.96±0.572 |
2.87±0.550 |
6.54±1.237 |
| (2.08–4.19) |
(2.08–3.99) |
(5.05–10.70) |
| Experimental group (n = 50) |
2.88±0.630 |
2.80±0.574 |
6.43±1.361 |
| (2.05–4.35) |
(2.05–4.31) |
(4.88–9.92) |
| P value |
0.590ns |
0.595ns |
0.685ns |
| (t value) |
(0.542) |
(0.535) |
(0.409) |
| At the end of study |
Control group (n = 50) |
3.00±0.551 |
2.90±0.522 |
6.37±1.291 |
| (2.04–3.95) |
(2.04–3.92) |
(5.23–10.43) |
| Experimental group (n = 50) |
3.20±0.675 |
3.05±0.554 |
7.20±1.612 |
| (2.11–4.53) |
(2.02–4.44) |
(4.96–11.84) |
| P value |
<0.05* |
<0.05* |
<0.05* |
| (t value) |
(2.019) |
(2.043) |
(2.541) |
Data are expressed as mean ± SD. Figures in parenthesis indicate range, statistical analysis conducted by using Student’s unpaired t-test, ns = not significant
* = statistically significant test (P < 0.05).
ANB, alternate nostril breathing; FVC, forced vital capacity; FEV1, forced expiratory volume in 1st second; PEFR, peak expiratory flow rate.
|
Table 2 Comparison of Respiratory Parameters between the Beginning and the End of the Study in Control (without ANB Exercise) and Experimental Group (with ANB Exercise) (n = 100)
| Respiratory |
Attributes |
FVC (Liter) Mean ± SD (Range) |
FEV1 (Liter) Mean ± SD (Range) |
PEFR (Liter/sec) Mean ± SD (Range) |
| Control group (n = 50) |
At the beginning of study |
2.96±0.572 |
2.87±0.550 |
6.54±1.237 |
| (2.08–4.19) |
(2.08–3.99) |
(5.05–10.70) |
| At the end of study |
3.00±0.551 |
2.90±0.522 |
6.37±1.291 |
| (2.04–3.95) |
(2.04–3.92) |
(5.23–10.43) |
| P value |
0.537ns |
0.683ns |
0.336ns |
| (t value) |
(0.621) |
(0.411) |
(0.971) |
| Experimental group (n = 50) |
At the beginning of study |
2.88±0.630 |
2.80±0.574 |
6.43±1.361 |
| (2.05–4.31) |
(2.05–4.31) |
(4.88–9.92) |
| At the end of study |
3.20±0.675 |
3.05±0.554 |
7.20±1.612 |
| (2.11–4.53) |
(2.02–4.44) |
(4.96–11.84) |
| P value |
<0.001** |
<0.001** |
<0.001** |
| (t value) |
(8.066) |
(6.798) |
(4.090) |
Data are expressed as mean ± SD. Figures in parenthesis indicate range, statistical analysis conducted by Student’s paired t-test. ns = not significant (P > 0.05)
** = statistically significant test (P < 0.001).
ANB, alternate nostril breathing; FVC, forced vital capacity; FEV1, forced expiratory volume in 1st second; PEFR, peak expiratory flow rate.
|
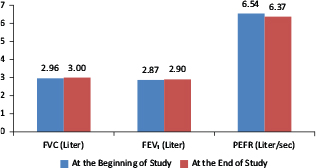
FIG 2. Respiratory Parameters in the Control Group (without ANB Exercise) at the Beginning and End of the Study.
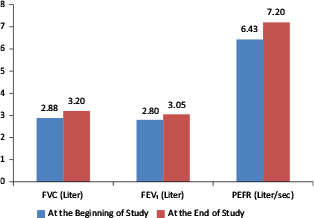
FIG 3. Respiratory Parameters in the Experimental Group (with ANB Exercise) at the Beginning and End of the Study.
DISCUSSION
This study assessed respiratory functions in the experimental group before and after ANB exercise for 4 weeks by analysis of FVC, FEV1, and PEFR values and compared these results with the control. In this study, for the control group, not practicing breathing exercises, the baseline values and the FVC, FEV1, and PEFR values after 1 month did not show any significant change. This finding is consistent with some previous studies conducted by Bal,9 Chanarivut et al.38 and Madanmohan et al.39 They also did not find any significant change in respiratory parameters in their studies.
In the experimental group that practiced ANB exercise for 1 month, mean FVC, FEV1, and PEFR were significantly increased from their baseline values. These findings are similar to those from some previous studies conducted by Biswas,2 Yadav and Das,7 Bal,9 and some other researchers.11,13,33–36,39,40–53 They supposed that FVC might be increased due to the strengthening of respiratory muscles by regular practicing of breathing exercises.2,42,44,45 FEV1 might be increased due to the removal of secretions from the bronchial tree, which made room in alveoli for more air after the breathing exercise.49 According to Raghavendra et al. yogic breathing involves isometric contraction and expansion of abdominal and intercostal muscles that may also improve the strength of intercostal muscles which lead to increased FVC and FEV1.54 Increased PEFR was supposed to be due to greater involvement of lung alveoli during the breathing exercise, which were dormant before the workout.41,50,55 According to Joshi et al.42 and Ankad et al.,51 PEFR were supposed to increase by increased release of lung surfactant and prostaglandins which reflexively relax the smooth muscle of the larynx and tracheobronchial tree. This modulates the caliber of the airways and reduces airway resistance which were the causal factors for increased PEFR in their study. According to Karmur et al.,11 Dhungel et al.,43 and Shrivastava et al.,56 increment in thoracopulmonary compliance and bronchodilatation by breathing exercise might be responsible for increased PEFR in their studies.57 In this study, improved respiratory functions after following the exercise for 1 month might be due to the above-mentioned causes.
Some investigators found only marginal improvement in FVC and FEV1 after pranayama training, which was dissimilar to this study.58,59 They explained that this might be due to a short period of research over which studies were conducted on normal healthy subjects.58,59 Alternate nostril breathing exercise brought significant improvement in respiratory parameters (FVC, FEV1, PEFR) in the experimental group of medical students.2,6 Therefore, ANB is very much helpful for the improvement of respiratory function as well as the prevention of different complications of respiratory problems.57 The limitation of this research was the fact that the study was conducted for both academic and clinical purposes over a short period of time. Although optimal care had been taken by the researcher in every step of the study, but there were some limitations: (1) short period of study, (2) small sample size that might not represent the whole community, (3) study was conducted with a limited age group, (4) the study was conducted on medical students of the first year only, (5) socio-demographic study could not be conducted, (f) proper sitting posture in the floor on the mat was not maintained, and (6) measurement of catecholamine level in blood and urinary excretion was not done to see the stress pattern.
CONCLUSION
In the present study, yoga-based ANB exercise done for a period of 1 month brought significant improvement in respiratory parameters (FVC, FEV1, and PEFR) in the study subjects. Though it was difficult to comment about the exact mechanism involved here, probably, it was due to shifting of sympathovagal balance towards parasympathetic predominance. Therefore, this study concludes that practicing ANB exercises can be a useful measure for the improvement of respiratory endurance and functions. This may help in preventing different complications of pulmonary problems in the future.
CONFLICT OF INTERESTS
The authors declare no conflict of interest.
FUNDING
This study received no financial support.
ACKNOWLEDGMENTS
The authors acknowledge the support of the Department of Physiology, CMC, Chattogram during sample collection and laboratory instrument uses. The authors are also thankful to the study subjects for their active, sincere, and voluntary participation.
DATA AVAILABILITY STATEMENT
The data will be available only for research purpose.
COMPLIANCE WITH ETHICAL STANDARDS
This study was approved by the Chittagong Medical College, Institutional Review Board, Bandladesh.
REFERENCES
- Sharma KK, Udayakumara K, Thirmaleshwara PH, Ajithesha NH. Effect of yoga therapy on lung functions in respiratory disorder subjects. Euro Sci J. 2014;10(6):102–8.
- Biswas S, Biswas P, Sayyad R, Eliyaraju A, Yadav PK, Kar SK. Effect of forty days of pranayama training on cardiorespiratory parameters. Indian J Basic Appl Med Res. 2014;3(4):196–202.
- Murray CJL, Lopez AD. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020 [Internet]. [cited 2019 Feb 11]. Available from: https://apps.who.int/iris/handle/10665/41864
- Hassan MR, Bennoor KS, Rahman F, et al. Prevalence of asthma in highly polluted Dhaka city and low polluted coastal area of Bangladesh. Indian J Allergy Asthma Immun. 2005;19(2):85–92.
- Alam DS, Chowdhury AH, Sidddique AT, Ahmed S, Clemens JD. Prevalence and determinants of chronic obstructive pulmonary disease (COPD) in Bangladesh. J Chronic Obstructive Pulmo Dis. 2015;2(1):1–11.
- Doijad VP, Kamble P, Surdi AD. Effect of yogic exercises on aerobic capacity. Int J Recent Trend Tech. 2013;6(3):119–21. https://doi.org/10.5958/j.2320-608X.1.2.010
- Yadav RK, Das S. Effect of yogic practice on pulmonary functions in young females. Indian J Physiol Pharmacol. 2001;45(4):493–6.
- Chethan K, Devaraju MR. A study on effect of nadi-shodhana pranayama on cardiac parameters. Indian J Basic Appl Med Res. 2016;6(1):484–7.
- Bal BS. Impact of short-term training of anulom vilom (alternate nostril breathing) on respiratory parameters. Am J Sports Sci Med. 2015;3(1):9–14. https://doi.org/10.269/ajssm-3-1-2
- Subhalakshmi NK, Saxena SK, Urmimala S, Urban JAD. Immediate effect of nadishodhana pranayama on some selected parameters of cardiovascular, pulmonary, and higher functions of brain. Thai J Physic Sci. 2005;18(2):10–16 [Internet]. [cited 2020 Jan 10]. Available from: https://www.researchgate.net/publication/24273802
- Karmur KA, Joshi VS, Maulik S, Padlia JL, Sarvaiya JL. Effect of ten weeks of yoga practice on pulmonary function tests. Int J Biomed Adv Res. 2015;6(9):682–5. https://doi.org/10.439/ijbar
- Pal GK, Agarwal A, Karthik S, Pal P, Nanda N. Slow yogic breathing through right and left nostril influences sympathovagal balance, heart rate variability, and cardiovascular risks in young adults. N Am J Med Sci. 2014;6(3):145–51. https://doi.org/10.4103/1947-2714.128477
- Chakraborti T, Das K, Samajdar K. Effect of yogic exercise on selected pulmonary function tests in apparently healthy elderly subjects. IOSR J Dent Med Sci. 2013;9(1):1–5. https://doi.org/10.9790/0853-0910105
- Ma X, Yue ZQ, Gong ZQ, Zhang H, Zhang H, Duan NY, et al. The effect of diaphragmatic breathing on attention, negative affect, and stress in healthy adults. Frontiers Psych. 2017;8(1):1–12. https://doi.org/10.3389/fpsyg.2017.00874
- Singh S, Katwal B, Panta PP. Slow and deep breathing exercise (pranayama) for a stress-free life amongst medical students. Int J Res Rev. 2017;4(7):67–72.
- Naik GS, Gaur GS, Pal GK. Effect of modified slow breathing exercise on perceived stress and basal cardiovascular parameters. Int J Yoga. 2018;11(1):1–14. https://doi.org/10.4103/ijoy.IJOY_41_16
- Telles S, Nagarathna R, Nagendra R. Breathing through a nostril can alter metabolism and autonomic activities. Indian J Physiol Pharmacol. 1994;38(2):133–7.
- Young MS, Lee YS, Lee HY. Effects of breathing exercise on resting metabolic rate and maximal oxygen uptake. J Physic Ther Sci. 2018;30(1):1173–1175. https://doi.org/10.1589/jpts.30.1173
- Shende V, Waghmore S, Pawar S, Kashalikar S. Effect of pranayama on blood glucose level in medical students: A case-control study. Int J Res Health Sci. 2013;1(3):209–12.
- Manjunatha S, Vempati RP, Ghosh RD, Bijlani RD. An investigation into the acute and long-term effects of selected yogic postures on fasting and postprandial glycemia and insulinemia in healthy young subjects. Indian J Physiol Pharmacol. 2005;49(3):319–24.
- Surendra BV, Hariprasad T. Effect of pranayama and yogasanas on lipid profile in normal healthy volunteers. Int J Clin Biomed Res. 2016;2(3):13–16.
- Chanda R, Sanjjev R, Rahul V, Mahapatra SP. Biochemical modulation in regular practice of yoga in young, healthy medical students. World J Pharmacy Pharmaceut Sci. 2017 Nov;6(2):617–28. https://doi.org/10.20959/wjpps201712-10520
- Shantakumari N, Sequeira S, Deeb RE. Effects of yoga intervention on lipid profiles of diabetes patients with dyslipidemia. Indian Heart J. 2013;65(1):127–31. https://doi.org/10.1016/j.ihj.2013.02.010
- Villemure C, Ceko M, Cotton VA, Bushnell MC. Neuroprotective effects of yoga practice: Age, experience, and frequency-dependent plasticity. Frontiers Human Neurosci. 2015;9(2):1–12. https://doi.org/10.3389/fnhum.2015.00281
- Subramanya P, Telles S. Effect of two yoga-based relaxation techniques on memory scores and state anxiety. Biopsychosoc Medi. 2009;1(1):1–5. https://doi.org/10.186/1751-0759-3-8
- Yadav G, Mutha PK. Deep breathing practice facilitates retention of newly learned motor skills. Nature Sci Rep. 2016;1(2):1–8. https://doi.org/10.1038/srep37069
- Berri K. Breathing to younger skin: ‘Reversing the molecular mechanism of skin aging with yoga.’ Future Sci OA. 2016;2(2):10–24 [Internet]. [cited 2020 Jan 10]. Available from: http://creativecommons.org/licenses/by/4.0/
- Sharma H, Datta P, Singh A, Sen S, Bhardwaj NK, Kochupillai V, et al. Gene expression profiling in practitioners of sudarshan kriya. J Psychosom Res. 2008;64(1):213–18. https://doi.org/10.1016/j.jpsychores.2007.07.003
- Pal GK, Velkumary S, Madanmohan S. Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120:115–21.
- Yadav RC. Effects of twelve weeks selected pranayama practice on primary high blood pressure patients. Euro J Pharmaceut Med Res. 2016;3(6):471–4 [Internet]. [cited 2020 Jan 10]. Available from: www.ejpmr.com
- Satyanand V, Kumar GPV, Ram NB, Mohanan D, Basha SA, Kumari BP. Study effect of two breathing techniques on pulmonary function in asthma. Int J Biomed Adv Res. 2014;5(8):510–12. https://doi.org/10.7439/ijbr
- Candy S, Singh S, Dandona PK. A study of the effect of yoga training on pulmonary functions in patients with bronchial asthma. Indian J Physiol Pharmacol. 2009;53(2):169–74 [Internet]. [cited 2020 Jan 10]. Available from: http://researchgate.net/publication/41187666
- Thirupathi C, Ananda SK. Effect of yoga exercise on pulmonary function in young medical students. Int J Medical Res Health Sci. 2016;5(11):341–3 [Internet]. [cited 2020 Jan 10]. Available from: www.ijmrhs.com
- Dhanvijay AD, Dhokne N, Choudhary AK, Kishanrao SS, Chandan L. Effects of alternate nostril breathing on cardiorespiratory variable in healthy young adults. Int J Pharmacy Biol Sci. 2015;6(2):1352–60 [Internet]. [cited 2020 Jan 10]. Available from: www.ijpbs.net
- Makwana K, Khirwadkar N, Gupta HC. Effect of short-term yoga practice on ventilator function tests. Ind J Physiol Pharmacol. 1988;32(1):202–8.
- Karthik S, Chandrashekhar M, Ambareesha S, Nikhil C. Effect of pranayama and suryanamaskar on pulmonary functions in medical students. J Clin Diag Res. 2014;8(12):4–6. https://doi.org/10.7860/CDR/2014/10281.5344
- Steps of Alternate Nostril Breathing (ANB) exercise [Internet]. [cited 2019 Feb 10]. Available from: www.medscapeonline.org
- Chanarivut R, Khaidjapho K, Jaree P, Prongnaratorn P. Yoga exercise increases chest wall expansion and lung volumes in young, healthy Thais. Thai J Physiol Sci. 2006;19(1):1–7.
- Madanmohan S, Jatiya L, Udupa K, Bhavani AB. Effect of yoga training on handgrip, respiratory pressures, and pulmonary function. Indian J Physiol Pharmacol. 2003;47(4):387–92.
- Doijad VP, Surdi AD. Effect of short-term yoga practice on pulmonary function tests. Indian J Basic Appl Med Res. 2012;3(1):226–30 [Internet]. [cited 2019 Feb 10]. Available from: www.ijbamr.com
- Gupta A, Gupta R, Sood S, Akram M. Pranayama for treatment of chronic obstructive pulmonary disease: Results from a randomized controlled trial. Integrat Med. 2014;13(1):26–31.
- Joshi LN, Joshi VD, Gokhale LV. Effect of short term ‘pranayam’ practice on breathing rate and ventilatory functions of lung. Indian J Physiol Pharmacol. 1992;36(2):105–8.
- Dhungel KU, Malhotra V, Sarkar D, Prajapati R. Effect of alternate nostril breathing exercise on cardiorespiratory functions. Nepal Med Coll J. 2008;10(1):25–7.
- Garg S, Chandla S. Effect of nadi shodhan pranayama on pulmonary functions. Int J Health Sci Res. 2016;6(4):192–6 [Internet]. [cited 2019 Feb 10]. Available from: www.ijhsr.org
- Shankarappa V, Prashanth P, Annamalai N, Varunmalhotra S. The short-term effect of pranayama on the lung parameters. J Clin Diag Res. 2012;6(1):27–30.
- Kumar K. Significance of nadi sodhan and kapalbhati on forced ventilation capacity (FVC), maximum voluntary ventilation (MVV), and peak expiratory flow rate (PEFR). Indian J Trad Knowl. 2013;12 (2):342–5 [Internet]. [cited 2019 Feb 10]. Available from: https://www.researchgate.net/publication/236119184
- Bal SB. Effect of anulom vilom and bhastrika pranayama on the vital capacity and maximal ventilatory volume. J Physic Educ Sport Manage. 2010;1(1):11–15 [Internet]. [cited 2019 Feb 10]. Available from: https://www.acadjourn.org/jpesm
- Panwar S, Chourishi A, Makwana J. Effect of pranayama (yoga) on pulmonary function test of young, healthy students. Int J Pharmac Biol Sci. 2012;3(4):12–16 [Internet]. [cited 2019 Feb 10]. Available from: www.ijpbs.net
- Surendra BV, Chidri SV. Impact of short-term yogic practice over ventilator functions in healthy individuals. Int J Healthcare Biomed Res. 2014;2(3):140–6 [Internet]. [cited 2019 Feb 10]. Available from: ijhbr.com
- Sivapriya DV, Suba-Malani S, Thirumeni S. Effect of nadi shodhana pranayama on respiratory parameters in school students. Rec Res Sci Tech. 2010;2(11):32–9.
- Ankad RB, Ankad BS, Anita H, Shailaja P, Surekharani C, Shashikala GV. Effect of short-term pranayama and meditation on respiratory parameters in healthy individuals. Int J Collab Res Intern Med Pub Health. 2011;3(6):10–14.
- Singh S, Gaurav V, Parkash V. Effects of a 6-week nadi-shodhana pranayama training on cardio-pulmonary parameters. J Physic Educ Sports Manage. 2011;2(4):44–47.
- Dullo P, Vedi N, Gupta U. Improvement in respiratory functions after alternate nostril breathing in healthy young adults. Pakistan J Physiol. 2008;4(2):15–16.
- Raghavendra P, Shetty P, Shetty S, Manjunath NK, Saoji AA. Effect of high-frequency yoga breathing on pulmonary functions in patients with asthma: A randomized clinical trial. Ann Allergy Asthma Immunol. 2016;117(5):550–551. https://doi.org/10.1016/j.anai.2016.08.009
- Gupta V, Singh Y, Vikramaditya B, Singh H. Immediate effect of “nadi-shodhana pranayam” on some selected parameters of cardiorespiratory and mental efficiency. J Curr Trends Clin Med Laborat Biochem. 2014;2(3):12–15.
- Shrivastava RD, Nidhi J, Singhal A. Influence of alternate nostril breathing on cardiorespiratory and autonomic functions in healthy young adults. Indian J Physiol Pharmacol. 2005;49(4):475–83.
- Saoji AA, Raghavendra BR, Manjunath NK. Effects of yogic breath regulation: A narrative review of scientific evidence. J Ayurveda Integr Med. 2019;10(1):50–58. https://doi.org/10.1016/j.jaim.2017.07.008
- Dinesh T, Gaur G, Sharma VK, Madanmohan T, Kumar KTH, Bhavani AB. Comparative effect of 12 weeks of slow and fast pranayama training on pulmonary function in young, healthy volunteers: A randomized controlled trial. Int J Yoga. 2015;8(1):22–6. https://doi.org/10.4103/0973-6131.146051
- Tarunker AV, Jain S, Patel SB, Sinha SR, Joshi AD, Vallish BN, et al. Effects of slow breathing exercise on cardiovascular functions, pulmonary functions & galvanic skin resistance in healthy human volunteers-a pilot study. Indian J Med Res. 2013;137(5):916–21.