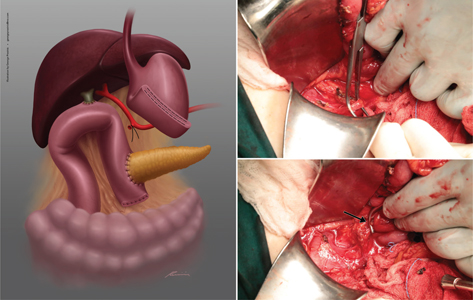
FIG 1. Ligation of the GDAS (Black Arrow). The Vessel is Ligated using PDS 3/0.
Research Article
Serafeim Klimopoulos1, Alexandra Charakopoulou1, Athanasios Pantelis1 and Konstantinos Bouchagier1
12nd Department of General Surgery, General Hospital of Athens “Evangelismos,” Athens, Greece
Post-pancreaticoduodenectomy hemorrhage has an estimated incidence of 5% and a mortality rate of 11–38%. Vascular erosion resulting from pancreatic leak and skeletonization of the arterial wall during pancreatic mobilization may be the two possible mechanisms responsible for this complication, which most commonly affects the gastroduodenal artery stump. A novel technique of wrapping up the gastroduodenal artery stump into the jejunal serosa to decrease postoperative hemorrhage is presented.
Keywords: pancreatic cancer; pancreaticoduodenectomy; post-pancreatectomy hemorrhage; gastroduodenal artery; pseudoaneurysm
Whipple procedure is the procedure of choice for the treatment of periampullary and pancreatic head malignancies. Although perioperative mortality has significantly decreased over the years (0–5% in high volume centers), morbidity still remains high (20–40%).1,2 The most common complications are pancreatic leak (40%), delayed gastric emptying (18%), wound infection (7%), intra-abdominal abscess (6%), and hemorrhage (5%).1–3
Post-pancreatectomy hemorrhage has a mortality rate of 20–50%.4 The International Study Group of Pancreatic Surgery defined post-pancreaticoduodenectomy hemorrhage on the basis of three objective parameters: time of onset (early hemorrhage that occurs within 24 h postoperatively and late hemorrhage occurring >24 h postoperatively), location (intraluminal or extraluminal), and severity (mild or severe).5 Technical issues and perioperative coagulopathy disorders are the predominant causes of early post-pancreatectomy hemorrhage, whereas the most common cause of late post-pancreatectomy hemorrhage is a pseudoaneurysm formation of the gastroduodenal artery stump, due to a leak from pancreaticojejunostomy (33%).6,7 Several techniques to prevent the erosion of the gastroduodenal artery stump and the subsequent post-pancreatectomy hemorrhage have been proposed, including the usage of the omentum, the falciform ligament, and the round ligament as serosal patches.
This report aims to introduce a new technique using the jejunal serosa to cover the gastroduodenal artery stump, so as to reduce post-pancreatectomy hemorrhage.
The patients underwent either Kausch–Whipple or Traverso–Longmire pancreaticoduodenectomy procedure. According to the standard technique, ligation of the Gastroduodenal artery stump (GDAS) was performed at the initial stage of the procedure (Figure 1).
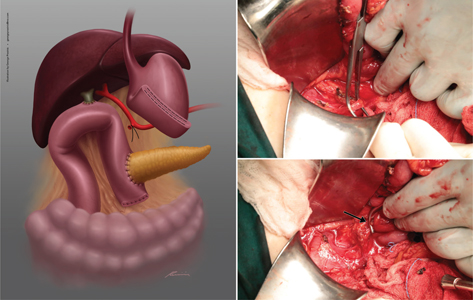
FIG 1. Ligation of the GDAS (Black Arrow). The Vessel is Ligated using PDS 3/0.
The highlight of our technique is the embedment of the gastroduodenal artery stump into the serosa of the jejunum at a point between the pancreaticojejunostomy and the choledochojejunostomy. Specifically, after standard ligation of the vessel with Polydioxanone suture (PDS) 3/0 and completion of the three anastomoses, the vessel is approximated to the jejunal serosa, in a tension-free fashion and is then fixed in an adventitia–serosa–adventitiamanner with three or four PDS 3/0 interrupted sutures, in a 360° single layer (Figures 2 and 3).
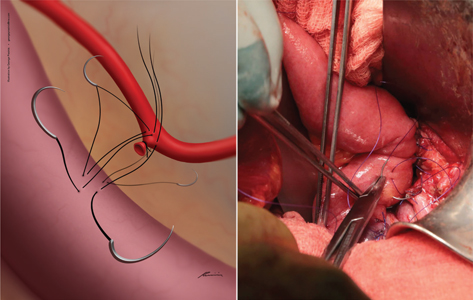
FIG 2. Suturing of the GDAS to the Jejunal Serosa. The gastroduodenal artery stump is approximated to the jejunal serosa in a tension-free fashion and fixed in an adventitia–serosa–adventitia manner with PDS 3/0 interrupted sutures in a 360° single layer.
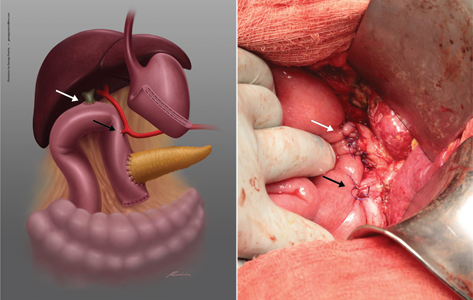
FIG 3. Gastroduodenal Artery Stump Embedment into the Jejunal Serosa (Black Arrow) Proximal to the Choledochojejunal Anastomosis (White Arrow).
A total of 51 patients underwent Whipple procedure with embedment of the gastroduodenal artery stump into the jejunal serosa. Forty-four percent of the patients were females and 56% were males, with a median age of 69 years (Table 1). A total of 42 patients had minor perioperative bleeding, which was transfused with two blood units, and nine patients had severe perioperative bleeding, which was transfused with more than four units of blood and clotting factors. Postoperative pancreatic fistula was confirmed in 11 patients, with a three-fold increase in the amylase levels of the drained fluid, compared with serum amylase levels, whereas 12 patients had delayed gastric emptying, postoperatively. The pancreas texture was soft in seven of these patients, whereas four patients had a hard pancreas texture. Nine patients presented with postoperative hemorrhage, which was treated through Penrose drains—three of them were treated conservatively with blood transfusion and clotting factors, five patients underwent an urgent laparotomy, and one patient underwent CT angiography, that set the diagnosis of splenic artery pseudoaneurysm. However, the “CT angiography” patient later underwent urgent laparotomy, due to uncontrollable bleeding, which caused severe hemodynamic instability. Among the patients that underwent urgent laparotomy, the gastroduodenal artery stump was found intact in all of them, while other bleeding sites were identified as bleeding sources, like retroperipancreatic vessels or splenic artery pseudoaneurysm. The median overall hospital stay was 32 days. Two patients died postoperatively (mortality = 3%)
| n = 51 | |
| Median age (SD) | 69 (64–75) |
| Sex | |
| Male | 29 (56.9) |
| Female | 22 (43.1) |
| SD = standard deviation. | |
Pancreaticoduodenectomy is a major surgical procedure performed for hepatobiliary and pancreatic malignancies.1–4 Pancreaticojejunostomy leak is the most morbid complication, which leads to intra-abdominal collections, abscesses, and erosion of the adjacent gastroduodenal artery stump, with subsequent postoperative hemorrhage.1–4 Risk factors for pancreaticojejunostomy leak are Table 2 the soft pancreatic texture, the undilated pancreatic duct, and the perioperative transfusion.1 Several methods have been described to diminish the risk of pancreaticojejunostomy leak, including the use of somatostatin or pancreatic stents; however, none of these techniques has been found to be effective.1 Omental patches and falciform ligament patches to wrap up the gastroduodenal artery stump have been described in the literature as effective techniques to reduce postoperative hemorrhage. The advantages of the omental patch are the excellent vascularity, the high capacity to absorb fluids, and neovascularization. The disadvantages are the intestinal obstruction due to adhesions, the development of panniculitis, and the creation of intra-abdominal abscesses.8–14
The aim of this article is to propose a new surgical technique of wrapping up the gastrointestinal stump into the jejunal serosa, to avoid the skeletonization of the gastroduodenal artery stump if a pancreaticojejunostomy leak occurs. The benefits of this novel technique are its simplicity and the fact that it can be done in a few minutes with significant results, as mentioned above. Moreover, it is cost-effective and safe, as no associated complications have been recorded.
In conclusion, this is a first description of this surgical technique, which aims to reduce the increased post-pancreaticoduodenectomy morbidity. However, randomized trials are mandatory to evaluate the possible benefits of this addition to the well-established procedure.
Prasinis George created the drawings that illustrate the novel technique of wrapping up the gastroduodenal artery stump into the jejunal serosa.