INTRODUCTION
Diabetes mellitus (DM) is a chronic metabolic condition marked by excessive blood glucose levels that damages various organs and tissues of the body, including the eyes.1 DM is classified into three major types: type 1, type 2, and gestational diabetes.2 The number of people affected with DM is rising in both industrialized and developing nations worldwide,3 with Saudi Arabia ranking seventh with a higher population, aged 20–79 years, having DM (a frequency of 24%).4 One of the microvascular problems associated with DM is diabetic retinopathy (DR), affecting about 24% of diabetic patients who had the condition for 10–15 years.5The overall pooled prevalence from different studies quote about 34.6% of the diabetic patients develop diabetic retinoipathy.6,7 DR is a retinal illness characterized by compromised oxygen and nutrition supply to the retina,8 causing vision impairment and blindness.9 Approximately 35% of diabetic persons worldwide develop DR since poor glycemic control is a major factor for DR.10 Given the nature of DM, the majority of patients were not aware of DR condition and sought treatment in later stages.11,12 Awareness and knowledge of DR are essential for early diagnosis, therapy, and avoidance of prospective vision impairment, which aids in retinopathy prevention strategies.13–15 Poor adherence to guidelines, delays in referral, and presentation with advanced DR can affect the patient’s quality of life and the financial costs to health systems if primary care physicians and their patients are unaware of DR, the importance of regular eye exams, and the benefits of treatment.16–18 The level of education, understanding, and adherence to DR among diabetic patients must be assessed given the growing rate of DM among Saudi Arabia’s population.19 This study assessed the level of public awareness and understanding of DR in Riyadh, Saudi Arabia.
MATERIAL AND METHODS
Study Design and Patients
This cross-sectional study was conducted between November 2021 and March 2022. The data on the awareness of DR was collected using a self-constructed questionnaire among primary DM patients. The participants included both male and female Saudi DM patients who visited primary care centers and were between 15 and 80 years of age. Patients who were not Saudi nationals, had congenital eye disease, had prior eye trauma, were known cases of or being treated for other eye diseases such as cataract or glaucoma, and had a history of cognitive impairment that made it difficult for them to complete the survey or follow instructions (e.g., mental retardation, dementia, psychosis) were excluded from this study.
Size of the Sample and Method
The sample size was calculated based on a predicted awareness of 88%, with a margin of error of 5% at a 95% confidence level. Following basic random sampling, 103 participants were chosen.
Statistic Evaluation
The data was analyzed using SPSS program version 26.0, where number and percent were used for qualitative variables, while mean and standard deviation (SD) were used for quantitative variables. The Chi-square test was used for univariate analysis; p < 0.05 was considered significant. The frequency command was used to illustrate the frequency table for variables, such as age, gender, and other sociodemographic characteristics, by frequency and percentage.
RESULTS
Of the participants, the age group most affected by DM was 51–60 years (32%), followed by 41–50 years and 31–40 years (both at 20.4%). The prevalence of DM was low among the population aged between 21 and 30 years (3.9%) (Figure 1).
FIG 1. Age distribution of study participants.
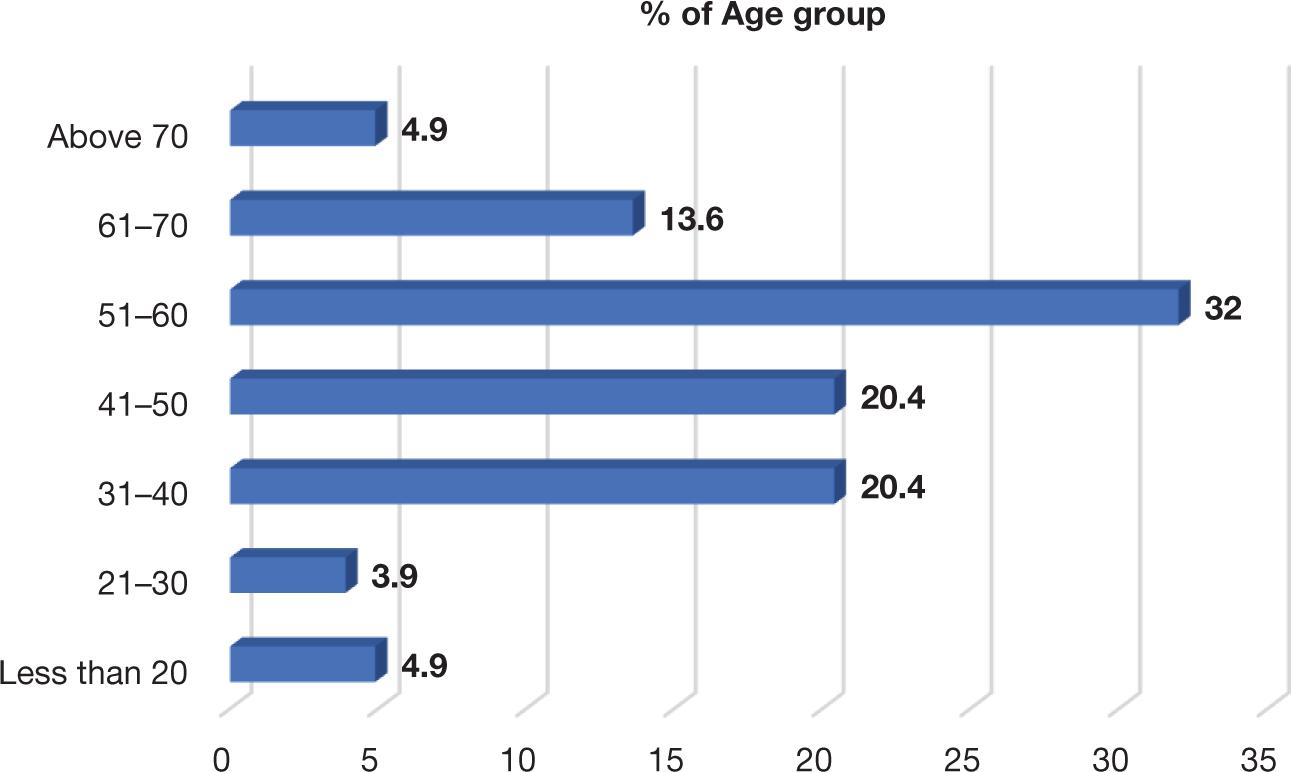
Figure 2 shows the duration of diabetes among the study participants. The mean number of years for patients with DM was 11.5 years and SD was 8.553, indicating that the number of years of prevalence of DM in patients was not a homogeneous distribution.
FIG 2. Frequency distribution of duration of diabetes among study participants.
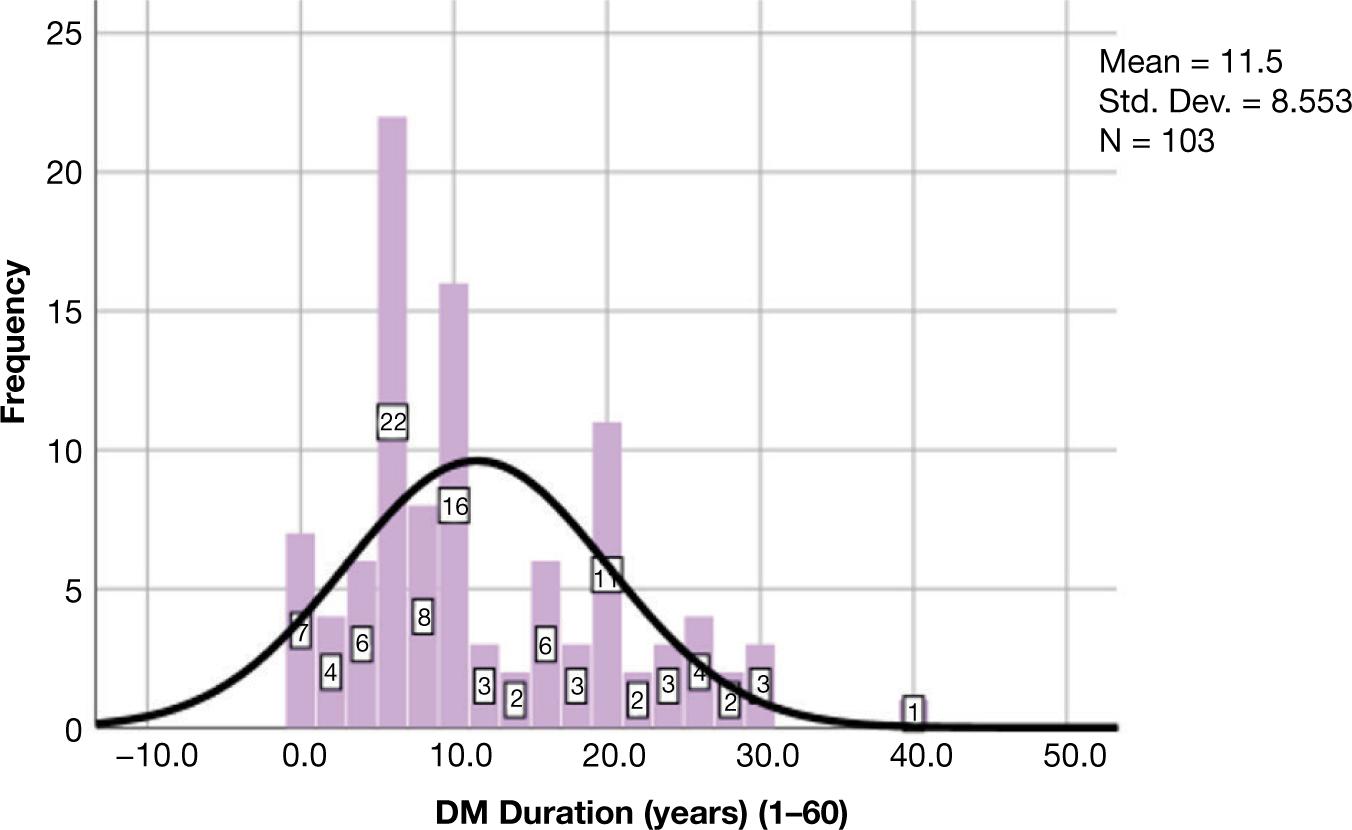
Of the 103 participants, 22 patients had the condition for 6–8 years, 16 patients had between 10 and 12 years, 11 patients between 20 and 22 years, only one patient had a 40-year DM diagnosis, and the rest had the condition lesser than 6–8 years.
Table 1 shows the degree of awareness among diabetic patients for DR. The majority of participants (79.6%) knew that DM causes DR while 20.4% remained unaware. Of the study participants, 16.5% reported that their knowledge of DR being a possible complication of diabetes was obtained from media, 46.6% from doctors, 1.0% from family, 4.9% from friends, and 11.7% from other diabetic patients, while 19.4% of them had no awareness. About 57.3% of the respondents reported that DM could cause blindness while 42.7% of them reported otherwise.
TABLE 1. Knowledge and practices among diabetic patients with regards to Diabetic Retinopathy.
| Diabetes can Cause Diabetic Retinopathy | Frequency | % |
|---|---|---|
| Yes | 82 | 79.6 |
| No | 21 | 20.4 |
| If yes, how you know about it? | ||
| Media | 17 | 16.5 |
| Doctors | 48 | 46.6 |
| Family | 1 | 1.0 |
| Friends | 5 | 4.9 |
| Other diabetic patients | 12 | 11.7 |
| Unaware | 20 | 19.4 |
| Do you know when you should screen | ||
| When I have a complaint | 68 | 66.0 |
| When I do not have complaint | 17 | 16.5 |
| Unaware | 18 | 17.5 |
| Do you think that diabetes could cause blindness? | ||
| Yes | 59 | 57.3 |
| No | 44 | 42.7 |
| DM can affect eye without affecting vision and needs treatment within time? | ||
| Yes | 58 | 56.9 |
| No | 44 | 43.1 |
| Diabetes can Cause Diabetic Retinopathy | Frequency | % |
| Did you consult an eye specialist before? | ||
| Yes | 64 | 62.1 |
| No | 39 | 37.9 |
| If yes, why? | ||
| I had a complaint | 48 | 46.6 |
| They told me the importance of screening | 16 | 15.5 |
| Unaware | 39 | 37.9 |
| Total | 103 | 100.0 |
Of the respondents, 56.9% of the respondents reported that DM could affect eye without affecting the vision, requiring treatment. Two-thirds (62.1%) of the patients had consulted an ophthalmologist earlier, while 37.9% of them did not. About half (46.6%) of the participants had consulted an eye specialist due to some related complaint, while 15.5% consulted an eye specialist as they highlighted the importance of screening.
Table 2 shows that out of 103 study participants, who consulted a specialist for management for DM-related eye complication, almost 26.2% (n = 27) received reassurance and control Blood Glucose(BG) with an annual follow-up. About 13.6% (n = 14) received reassurance and control BG with a 6 monthly follow-up routine. However, 37.9% (n = 39) received no management at all. Of the consulted patients, 3.9% (n = 4) received laser treatment and 2.9% (n = 3) received surgery while 1.9% received laser treatment along with an injection in the eye.
TABLE 2. Percentage distribution of patients who received different management modalities from the specialist.
| Different Treatment Modalities Received by Diabetic Patients | Frequency | % |
|---|---|---|
| Reassurance and control BG and annual follow-up | 27 | 26.2 |
| Reassurance and control BG and follow-up every 6 months | 14 | 13.6 |
| Reassurance and control BG and follow-up every 3 months | 3 | 2.9 |
| Laser treatment | 4 | 3.9 |
| Injections in eye | 11 | 10.7 |
| Surgery | 3 | 2.9 |
| Laser and injection in eye | 2 | 1.9 |
| Answered no | 39 | 37.9 |
| Total | 103 | 100.0 |
Table 3 shows the treatment modalities for DR. The majority of respondents (68.0%) were not aware of any kind of treatment modality for retinopathy. Of the patients who had medical consultation, 5.8% reported laser treatment, 4.9% for eye injection, 6.8% for surgery, and 14.6% for both laser and injection in the eye.
TABLE 3. Distribution of participants’ awareness of various treatment modalities for DR.
| Awareness Among Diabetic Patients with Regards to Different Treatment Modalities for Diabetic Retinopathy | Frequency | % |
|---|---|---|
| I do not know | 70 | 68.0 |
| Laser | 6 | 5.8 |
| Eye injection | 5 | 4.9 |
| Surgery | 7 | 6.8 |
| Laser and injection in eye | 15 | 14.6 |
| Total | 103 | 100.0 |
DISCUSSION
This cross-sectional, self-constructed questionnaire study conducted at primary healthcare centers of Al-Kharj, Saudi Arabia reflected the awareness of DR among DM patients. The age group most affected with DM (32%) was 51–60 years, followed by 41–50 and 31–40 years (both 20.4%). The least affected (3.9%) were the subjects between 21 and 30 years of age. The mean number of years in patients with DM was 11.5 years, with an SD of 8.553, indicating that the number of years of prevalence of DM in patients was not a homogeneous distribution. Of the 103 participants, 22 patients had the condition for 6–8 years, 16 patients had between 10 and 12 years, 11 patients between 20 and 22 years, only one patient had a 40-year DM diagnosis, and the rest had the condition lesser than 6–8 years.
Only 47.6% of diabetic patients were diagnosed by a regular check-up within 3–6 months. Screening for diabetes should begin at 45 years of age in the absence of other risk factors, such as high body mass index or hypertension, according to the 2015 clinical practice guidelines of the American Association of Clinical Endocrinologists and the American College of Endocrinology.20 In this study, almost all patients (79.6%) believed that diabetes could affect the eye, which was consistent with the findings of Al Zarea,21 who reported that 75.62% of diabetic patients visiting hospitals and primary care centers in Saudi Arabia’s AlJouf and Hail provinces were aware that diabetes could cause eye disorders, and Cetin et al.,22 who discovered that DR awareness among diabetic patients was high. The studies conducted by Liu et al.23 in urban diabetic patients in China and Ahmed et al.24 in diabetic patients visiting tertiary care hospitals in Bangladesh revealed that a significant percentage of study participants, 36.6% and 63%, respectively, were aware of retinopathy as a diabetic complication of the eye, resulting in blindness. This result is higher than this study’s finding (57.3%), which could be due to cultural differences.
Almost all the patients in this study believed that diabetes could harm their eyes, as most of the patients were hospitalized, where they may have heard about the possibility of DM-related eye complications. Only 26.2% had a regular eye examination, which was consistent with the above-mentioned study at a tertiary care hospital in Bangladesh, where only 49% were aware of the need for periodic eye examinations for DR, with only 37% reported having done so annually.24 The lack of knowledge and awareness of DR, the chronic nature of DR, and the long latent period of symptom manifestations are the contributing factors for not consulting medical professionals. Only 37.9% of the study participants had never seen an ophthalmologist, which was similar to a study conducted by Ogbomo et al.,25 at Ghana’s Korle-Bu teaching hospital, where only 34.5% had not seen an ophthalmologist after being diagnosed with diabetes.
CONCLUSION
This study showed the degree of awareness of DR among DM patients. The majority of study participants (79.6%) believed that DR can be a possible complication of DM. Out of these patients, 16.5% obtained this information from the media and 46.6% from specialist doctors. The majority (66.0%) opined to consult ophthalmologist if they had visible symptoms, while more than half (57.3%) reported that DM could cause blindness. More than half of the study population (56.9%) reported that DM could affect the eye without affecting vision, requiring treatment. Two-thirds (62.1%) consulted an ophthalmologist earlier, with 46.6% consulting due to some complaint. The majority (68.0%) had no idea about various treatment modalities for DR. These results cannot be externally validated for all diabetic patients who did not suffer from any complaints and did not visit any healthcare facility or specialist clinics, which is the limitation of this study.