INTRODUCTION
At present, the treatment of local defects and diseases of the meniscus of the knee joint is one of the most urgent and insufficiently studied problems in modern arthrology. During arthroscopy, in 63% of patients who undergo surgery, damage to the cartilage is determined 1,2
It is also believed that from the age of 30–40, on the surface of the meniscus of the knee joint (especially in the loaded areas), signs of age-related development are found—fibrillation (fibrillation), and with more detailed, microscopic examination, multiple fractures, and cleavage are found.3 Accordingly, a violation of the structure and function of the articular cartilage leads to pain, a decrease in the range of motion, deformation of the knee joint, and, eventually, as a consequence, to pronounced degenerative changes—to a gradual loss of cartilage tissue and irreversible articular changes.4,5
Multiple discussions and efforts of surgeons in the field of meniscus surgery have led to the introduction of a wide range of surgical interventions, microfractures, Autologous osteochondral mosaicplasty, and individual culture transplantation of chondrocytes.6–8
However, many issues of arthroscopic surgery of the knee joint and reconstructive treatment after surgery remain undiscovered and require close research due to the diversity of opinions in publications of the domestic and international literature (Korolev, 2004). In particular, opinions about arthroscopic methods of treating local defects of cartilage tissue in the knee joint are very controversial.9,10
Currently, in our country, there is no established system of indications and contraindications for all of the above-mentioned arthroscopic interventions in the presence of a local defect in the cartilage of the knee joint. In addition, there is no clear idea of the possibilities of innovative methods in this field.11 Generally accepted tactics for postoperative management and rehabilitation therapy for patients have not yet been developed.12 The immediate and long-term outcomes of arthroscopic treatment of localized cartilage defects of the knee joint have not been adequately studied. All this testifies to the importance of the topic chosen for this study, its theoretical and practical importance, which in turn served as the basis for its implementation.13
MATERIAL AND METHOD
Patient Sample
A study was carried out on 100 patients between the age of 40 and 70 years who underwent surgery for microfractures of cartilaginous knee lesions, where demographic information was collected for patients from Al-Anbar Hospital in Iraq to know the clinical changes that occurred after surgery.
Study Design
A retrospective study was conducted on patients who underwent minimally invasive surgery for the exact fracture of cartilaginous knee lesions. This study was conducted between 2017 and 2021, and the age of the patients ranged between 40 and 70 years in the Anbar Governorate.
It was considered that the patient was missing for the follow-up if he/she was called twice over the phone to visit the hospital to collect data and he/she did not show up. The patients’ initial information, their body mass index, and weight, in addition to the time they took to follow-up, was withdrawn. The hospital record contains information on the extent and location of cartilage abnormalities.
A distinct technique of employing microfractures and mosaic self-straightening was used to evaluate the quality of arthroscopic treatment of patients with localized cartilage abnormalities in the knee joint.
During the study, a global scale for the functional assessment of the knee joint was developed, which makes it possible to introduce this method into the practice of orthopedists involved in knee arthroscopy.
An endoscopic examination of patients should be carried out not only for timely local diagnosis but also for surgical repair of defects in the cartilage tissues of the knee joint.
Timely diagnosis and a clear and specific system of indications for arthroscopic tunneling, microfractures, and meniscal arthroplasty make it possible to carry out effective surgical and rehabilitation procedures that contribute to the early restoration of the function of the knee joint.
Study Period
With the cooperation of relevant committees to obtain licenses for this study, the information and demographic data were collected for the patients who underwent minimally invasive surgery to the exact fracture of cartilaginous knee lesions in the hospital for the period from February 2017 to August 2021.
Aim of Study
The purpose of this study is to evaluate the outcomes of arthroscopic microfracture for localized full-thickness cartilage abnormalities of the knee in Iraqi patients.
RESULTS
TABLE 1. Demographic results of patient.
| Variable | Value |
|---|---|
| Age, years (mean ± SD) | 49.8 ± 5.4 |
| Sex, N | |
| Male | 60 |
| Female | 40 |
| BMI, kg/ | 27.8 ± 3.7 |
| Follow-up duration (year) | 3.5 ± 0.8 |
| Defect size (cm2) | 3.6 ± 1.2 |
| Concomitant procedure, N | |
| Medial meniscectomy | 36 |
| Lateral meniscectomy | 19 |
| Medial and lateral meniscectomy both | 15 |
| None | 30 |
| Location of lesion | |
| Lateral femoral condyle | 55 |
| Fossae | 30 |
| Multiple | 15 |
FIG 1. Distribution of patients according to the follow-up period (year).
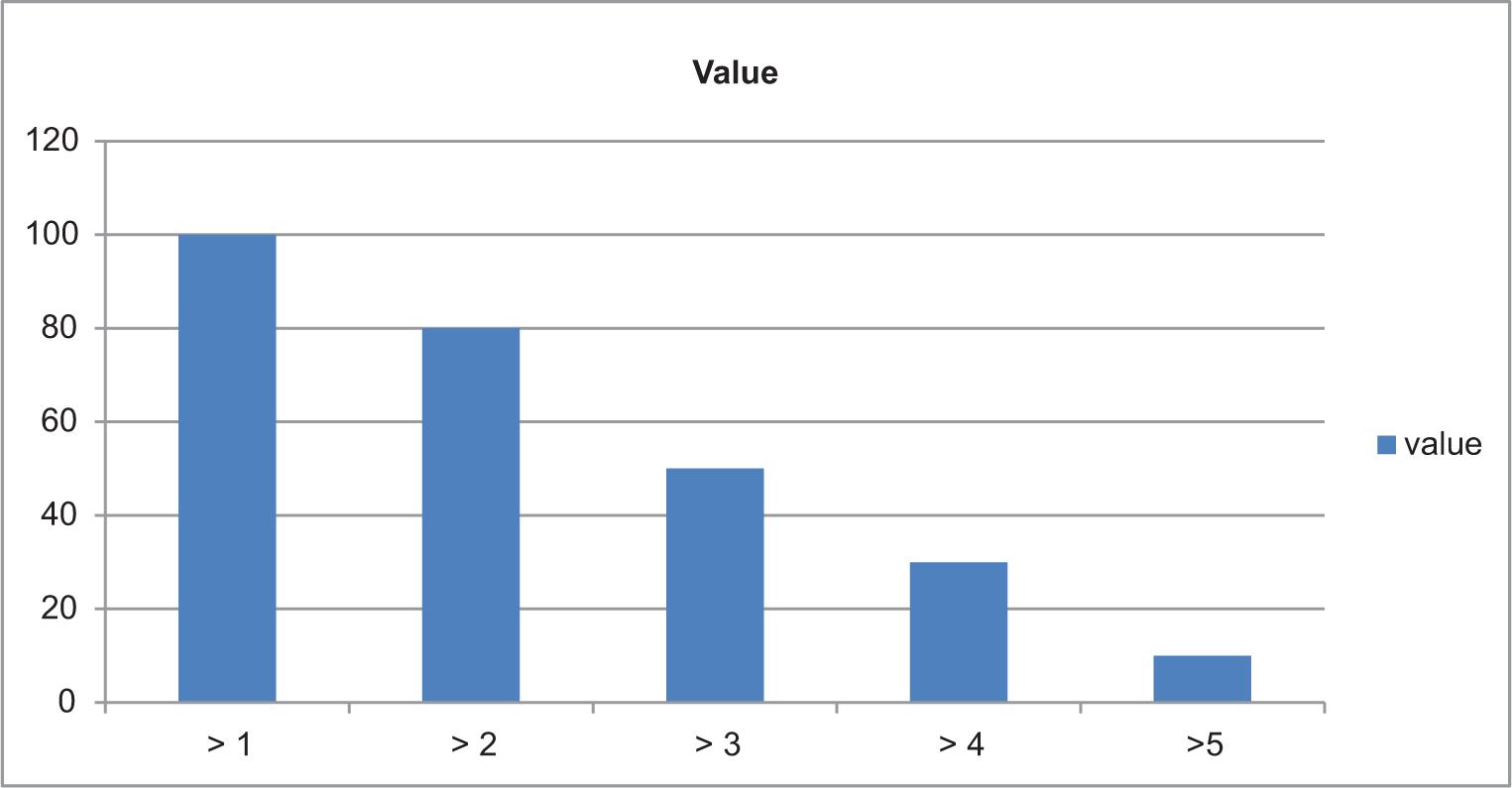
FIG 2. Clinical trend analysis of patients undergoing microfracture according to KOOS, Lysholm, Tenger, and pain VAS.
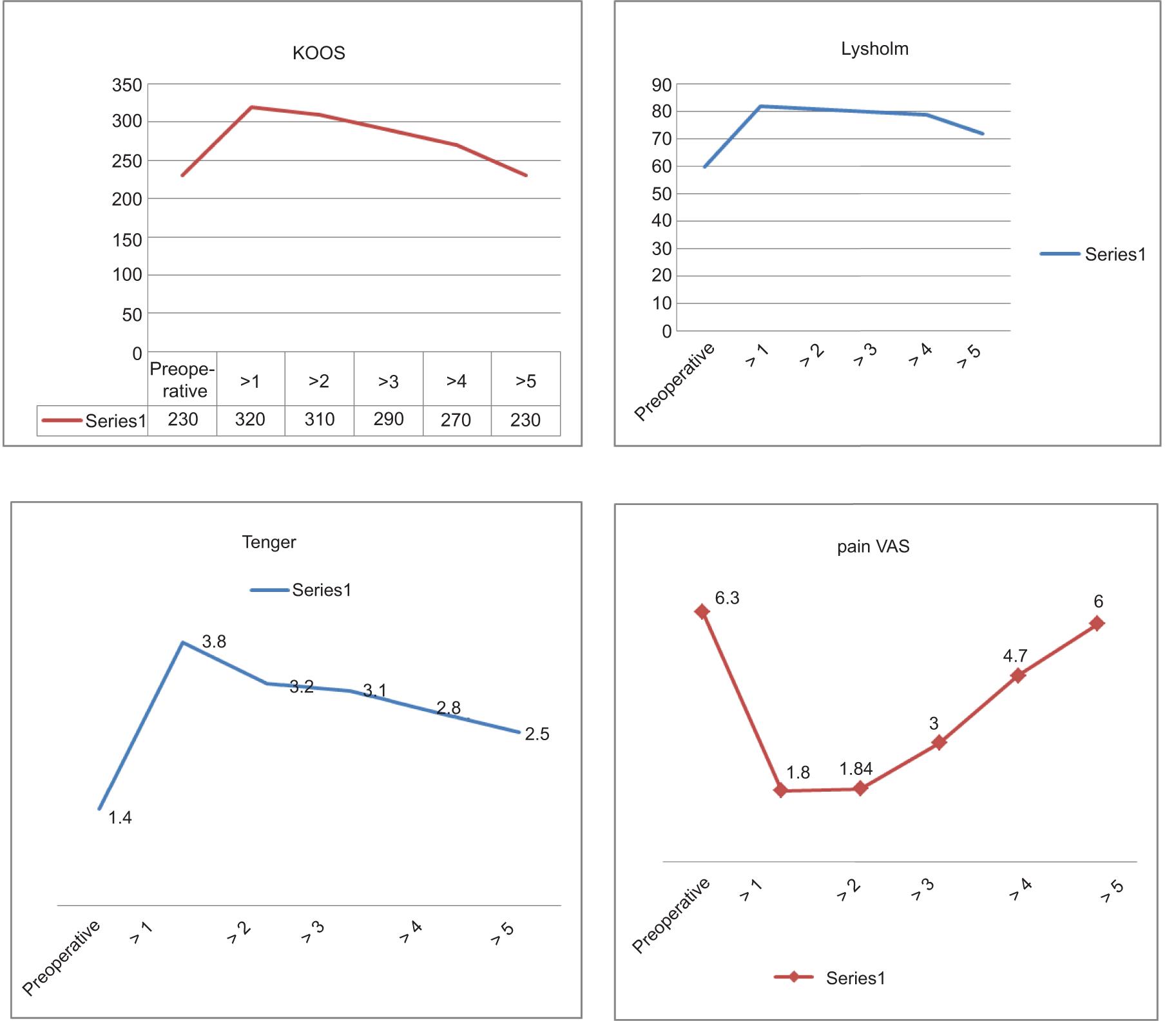
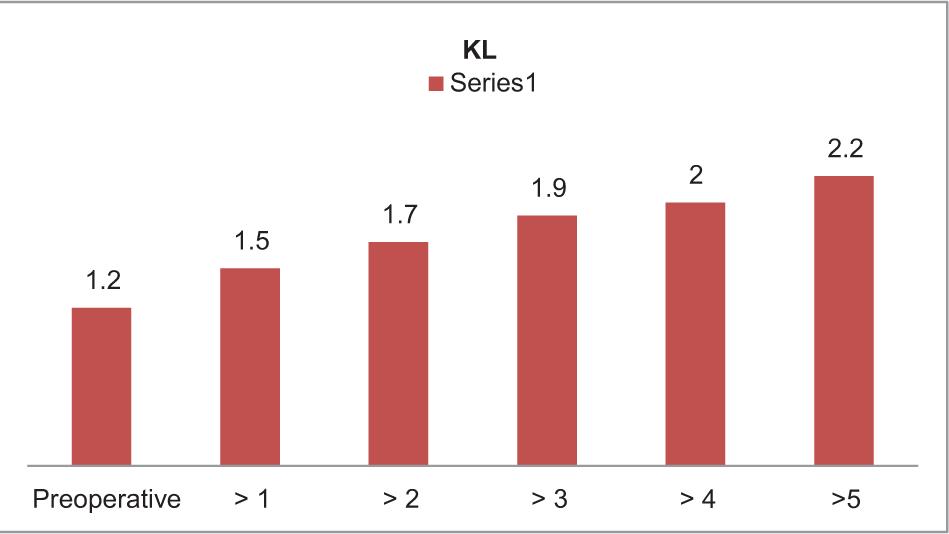
FIG 3. Outcomes of radiological evaluation according to KL grade.
DISCUSSION
In this study, data from 100 patients were collected, and a statistical analysis program, IBM SPSS soft 22, in addition to Microsoft Excel 2013, was used to analyze the data, the demographic information of patients, and the real value and the arithmetic mean of the patient’s age was 49.8 ± 5.4.
Patients were distributed according to gender (60 males and 40 females).
The results of this study were analyzed by the follow-up from 1 to 5 years. The most common concomitant procedure in patients was medial meniscectomy for 36 patients, none 30, lateral meniscectomy for 19 patients, and medial and lateral meniscectomy both for 15 patients.
A significant increase in the body mass index was observed in elderly patients over the age of 60 years, as shown in Table 1.
This study aimed to evaluate a clinical trend analysis of patients undergoing microfracture according to KOOS, Lysholm, Tenger, pain VAS.
The results showed a significant improvement in patients between the ages of 40 and 50 years, even after 5 years of surgery, and the clinical scores at 1 and 2 years were higher compared to the results before surgery.
In Figure 3, the results were evaluated according to the KL score, where stable scores were found even after 3 years after surgery.
Several studies similar to ours were found, as in Ranthamn (2001), where data from 302 patients with ages ranging from 20 to 35 years were collected.14,15
In other studies, such as Rayne Corsan (2001) in Canada, data from 139 patients were collected and classified according to gender, 80 male patients and 59 female patients. In this study, it was revealed that advancing age leads to the presence of arthritis and that over time, the survival rate increases with 2% of patients over 60 years of age.16
CONCLUSION
This study assessed the results of arthroscopic microfracture for localized full-thickness cartilage defects of the knee in patients from Iraq. The results showed a remarkable development in patients after 1 year, and this is due to several reasons, including advanced age, which is linked to a direct relationship with the poor results in this study.
RECOMMENDATIONS
-
Replacement of the defects of the articular surface of the knee joint with localized ones with limited space (not more than 2–4 cm), traumatic injuries of cartilage without obvious degenerative changes, or dissection of osteochondrosis or osteochondrosis should be performed by the method of autologous osteochondral grafts with cylindrical bone and cartilage autografts with strict adherence to the conditions for the stability of the knee joint and the integrity of the capsular ligament apparatus.
-
Localized cartilage defects with III- and IV-degree Y chondromalacia, which range from 4 to 6 cm, is the preferred method for microfracture, as microfractures must be performed at a certain depth (about 4 mm) with a Stedman awl/perforator in an amount of 3–4 per cm2 until the “bloody” content of the subchondral bone is released, which in turn leads to perforation of the bone and restoration of the defective integrity of the cartilage of the knee joint.
-
The versatility and practical ease of use of the Knee Joint Functional Assessment Scale developed in the course of the study make it possible to introduce this method into the practice of orthopedists involved in knee arthroscopy.